TRUST AS CURRENCY
Building trust and
changing lives with the
Intensive Outpatient Clinic



TRUST AS CURRENCY
Building relationships and changing lives with the Intensive Outpatient Clinic
By Stephen Dark
Portrait Photography by Louis Arévalo
December 20, 2021
When Adolphus Nickleberry woke up in hospital, he had an IV in his arm and an intubation tube down his throat. He was restrained by his wrists to the bed. A doctor looked down at him. “Welcome back,” the doctor said. “Again.”


TRUST AS CURRENCY
Building relationships and changing lives with the Intensive Outpatient Clinic
By Stephen Dark
Portrait photography by Louis Arévalo
When Adolphus Nickleberry woke up in hospital, he had an IV in his arm and an intubation tube down his throat. He was restrained by his wrists to the bed. A doctor looked down at him. “Welcome back,” the doctor said. “Again.”
It was the fifth time in November 2018 alone that Adolphus had visited the ER at University of Utah Hospital in Salt Lake City. Each time an ambulance had to be called because the 58-year-old had collapsed in respiratory failure after smoking crack cocaine, his emphysema-damaged lungs unable to get oxygen into his blood stream with the addition of the toxic smoke.
The drug user and dealer had been found barely breathing on State Street where, for 30 years, he’d been addicted not only to crack but also the hustle and drama of street life. He idly calculated spending $1 million on crack, and now all he had to his name was an oxygen tank to help with chronic obstructive pulmonary disease (COPD), a pipe, and a lighter.
“Man, what are you doing?” he thought. “This life ain’t me. I want my own apartment, my own car. I want my family back in my life.”

Ryan Morgan, a licensed clinical social worker at University of Utah Health’s Intensive Outpatient Clinic (IOC), learned Adolphus was in the ER the day after he was admitted. The IOC provides long-term medical and mental health care tailored to the individual needs of marginalized and impoverished patients who have lengthy, complex histories of addiction and trauma. Traditional clinics struggle to care for patients like Adolphus, so they end up repeatedly going to the ER or the hospital, placing a significant financial and medical drain on the health care system.
Adolphus wanted to return to a treatment center he’d done several stints at before. But when Morgan asked the center, they said their wait time was a year.
Morgan knew that Adolphus couldn’t wait that long. He called a director at the treatment center. “Adolphus is in the ED again,” Morgan said, a note of urgency in his voice. “We're afraid he's gonna die.” There was silence on the other end of the line. “Have him come here Saturday.”
COMMON GROUND

Adolphus Nickleberry and the Intensive Outpatient Clinic have much in common. Both struggled with difficult beginnings. Both survived by upending everything they had known—whether shutting the door on a way of life ingrained by decades of survival on the street or turning their backs on a health care system built on reimbursements of 15-minute increments that left no room to engage with patients unable to jump through hoops to receive their treatment. Both were driven by deeply personal goals: Peter Weir, MD, the IOC’s founder and executive medical director of population health at University of Utah Health, wanted to fundamentally change health care by addressing gaps in care. Adolphus wanted to become the caring parental figure his tragic childhood and addiction denied his children.

To reach those goals, both found themselves navigating sometimes surprising and certainly challenging byways of new worlds.
The IOC developed an approach to caring for marginalized patients that went against the fundamental grain of the bottom line that drives modern medicine. Instead of short interactions with patients that offered very little time for developing a relationship after the initial consult, IOC providers devoted hour-long appointments to each patient—and then remained connected with them after they left the clinic and went on facing their life challenges. The IOC pursued controversial approaches: a harm reduction model to addiction, which provides additional tools for providers working with patients unable or unwilling to stop substance use, along with an integral mental health model where social worker and medical provider had equal voice and footing in the team.

Adolphus had to learn to step out of his street role as a hustler who trusted no one to open himself up to the point of vulnerability so his IOC team could help him. He also had to find it within himself not only to stick to his commitment to sobriety but to learn to listen to his own instincts when he knew what was best for his recovery—even if it flew in the face of what he was being told by a treatment center or the IOC. That also meant seeking out mentors in the clinic and within the very family whose love he had long lost but hoped one day to earn back.
Ultimately, their journeys were indelibly intertwined. Adolphus and the IOC both had to prove that they could live up to their own promises of profound change.
GROWING PAINS

A quiet, polite man with a deeply rebellious, even subversive streak, Peter Weir invested everything in the IOC’s success. His passion lies in rethinking health care so it can be patient-focused, affordable, and accessible. He wanted his clinic to focus on patients who constantly struggled to engage with the health care system because trauma, mental health, addiction, and poverty got in the way of their intentions to seek help—and in the way of providers trying to deliver that help. These patients are difficult to treat and disruptive to a clinic’s workflow, adding to provider burnout. As a result, they rarely received the care they needed.

Weir’s initial idea was to bring “a very physician-centric mind frame,” he said, “namely that we’re going to find medically fragile people” and look at coordination of care to help them improve. University of Utah Health Plans agreed to fund the clinic through its Healthy U Medicaid program in exchange for bringing down the costs of some 100 Salt Lake County residents who, as identified through claims data, were consuming significant health resources through repeated visits to the ER and subsequent hospitalization. From the get-go, there was skepticism. When Weir told one doctor how the model worked, she laughed him out of her office.

The clinic opened in February 2017 in the basement of University Hospital, manned by a part-time medical provider, social worker, case manager, and assistant. Six months later, Weir knew he was onto something when the IOC’s first social worker told him something surprising: every IOC patient had a history of childhood trauma.
Weir thought it was “a crazy coincidence,” but his social worker shook her head. “There’s no such thing as coincidence,” she said. Childhood trauma made the IOC’s patients far more vulnerable to high-risk behaviors, poor compliance with taking medication and attending appointments, and histories of homelessness, incarceration, and poor nutrition.

A second theme emerged to link the IOC’s patients together: staying with them long-term and never giving up on delivering individualized care and support. “Our clinic is designed in every way to earn and develop trust with our patients,” Weir said. What helps to build that trust is what mainstream medicine doesn’t offer: home visits and working with patients to address substance abuse rather than demanding sobriety.
“That's our currency,” Weir said. “Trust is what gets the relationship going.”
WANTING TO BELONG


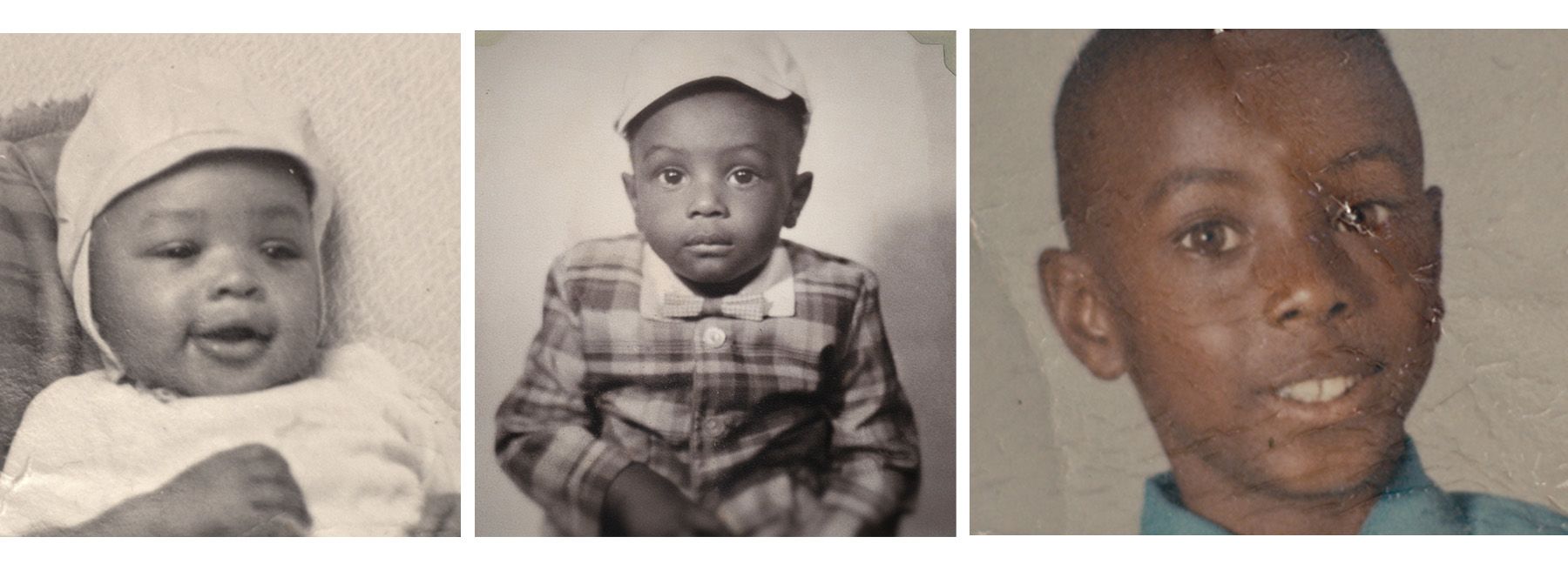
Childhood trauma was something that Adolphus knew intimately. Born in Salt Lake City, he grew up in the Rose Park neighborhood, close to Jackson Elementary where he attended kindergarten. Adolphus adored his mother, Jessie Lee, who had sickle cell anemia and stayed at home to care for her four children. His father, Adolphus Sr., struggled with asthma. He cleaned downtown offices at night, sometimes with his children helping by emptying wastepaper baskets while their father mopped and buffed floors.


As Jessie Lee got sicker, she couldn’t care for herself. One day when she needed to urinate, 5-year-old Adolphus tried to put the bedpan under her but was too late. That wasn’t the only memory that haunted him. He didn’t say goodbye to her. The first grader came home from school one day in June 1967 to find his 35-year-old mother’s bed empty. She had been taken to University Hospital. The next time he saw her, she was lying in a funeral casket, her face covered by a veil.
Three years later, tragedy struck again. One cold night in January 1969, when Adolphus was 8 years old, his 53-year-old father came home from work, entering uncharacteristically by the front door. He had had a severe asthma attack. “Should we call Dr. Bailey?” his father's brother asked, but their father said no. Doctors were expensive.
The next morning, their uncle went to check on his brother. “He’s passed away,” he said. Without a male role model, Adolphus latched on to an older brother, who used drugs, partied, and had gone to prison. “That’s my way of life,” Adolphus thought.
Grief wasn’t the only factor that shaped his youth—so did the racism he encountered in Utah growing up. At his nearly all-white junior high, Adolphus played basketball and ran track and field but found he fit in best with the students who skipped school and smoked weed—“the chosen few,” as he called them. Nevertheless, racial tension and fights were never far away. When a student called him a racist name, his friends said, “Man, take care of that, do something about it.” He fought constantly.

By the time he was 15, “the chosen few” had gone from fighting white kids to Pacific Islander youth. One day, to impress his friends, Adolphus took his grandfather’s gun to school. He pulled it out when someone gambling with his friend refused to pay a debt. A school cop appeared and Adolphus took off running, only to be arrested shortly after. He was court-ordered to an adolescent treatment program, but as soon as he finished the program, he was using drugs again.
BEHIND BARS

When he was 19, Adolphus started dating 17-year-old Audrey Drawn. She loved the color of his eyes and his smile. He was the best person you ever wanted to know, Audrey thought, who would give you anything and everything. But once he started drinking, he changed. If somebody talked to her, he clenched his fists; if somebody looked at her, he threw punches.
After Audrey graduated from East High School, she went to Westminster College and studied child psychology. Then she had her son James and, as she’d say, “real life started.” She and Adolphus became a family in the late 1970s, but when the 25-year-old Adolphus began using crack cocaine, that relationship came under constant pressure, both from his days-long absences binging drugs and his stints in jail. By then, he’d become addicted to “rippin’ and runnin’,” as he called his life on the streets. He dealt drugs to finance his own habit and, in the process, became known on State Street, North Temple, and downtown for his drug contacts—an uncrowned king of the streets who could always deliver the dope you needed if you had the cash.
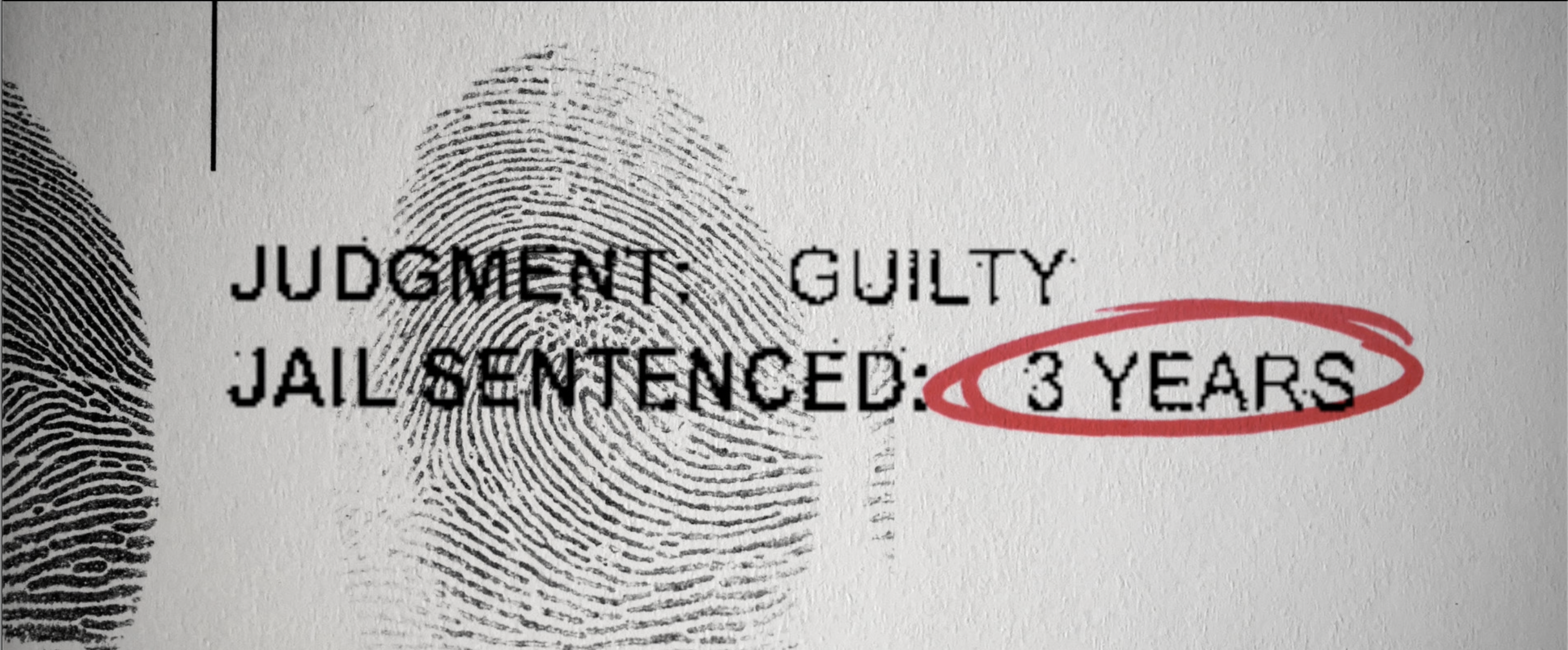
When Adolphus was arrested and jailed for drug-related offenses, Audrey went to see him, depositing money in his jailhouse account and talking to him on the phone. She was pregnant with their first child and wanted him to remember that his family was waiting for him on the outside. That summer of 1985, a different family called him. In jail awaiting trial on a retail theft felony, Adolphus met an old neighborhood friend, Ronnie Lee Gardner.
“Man, come to the joint,” said Gardner, who would soon be on death row for murder; decades later, he was executed by firing squad. Gardner reeled off familiar names from the neighborhood. “We’re all out there.” Rather than fight his charges, Adolphus took a plea deal so he could go to prison and be with his friends. Audrey was left alone to support James, baby Candice, and, subsequently, Aubrey, whom she had with another partner.
Adolphus got out of prison in 1987 and went to a halfway house, only to take off and start using again. He’d be gone for two or three days on a drug binge, then return home wanting only to sleep, any noise the children made earning his sharp-tongued criticism.
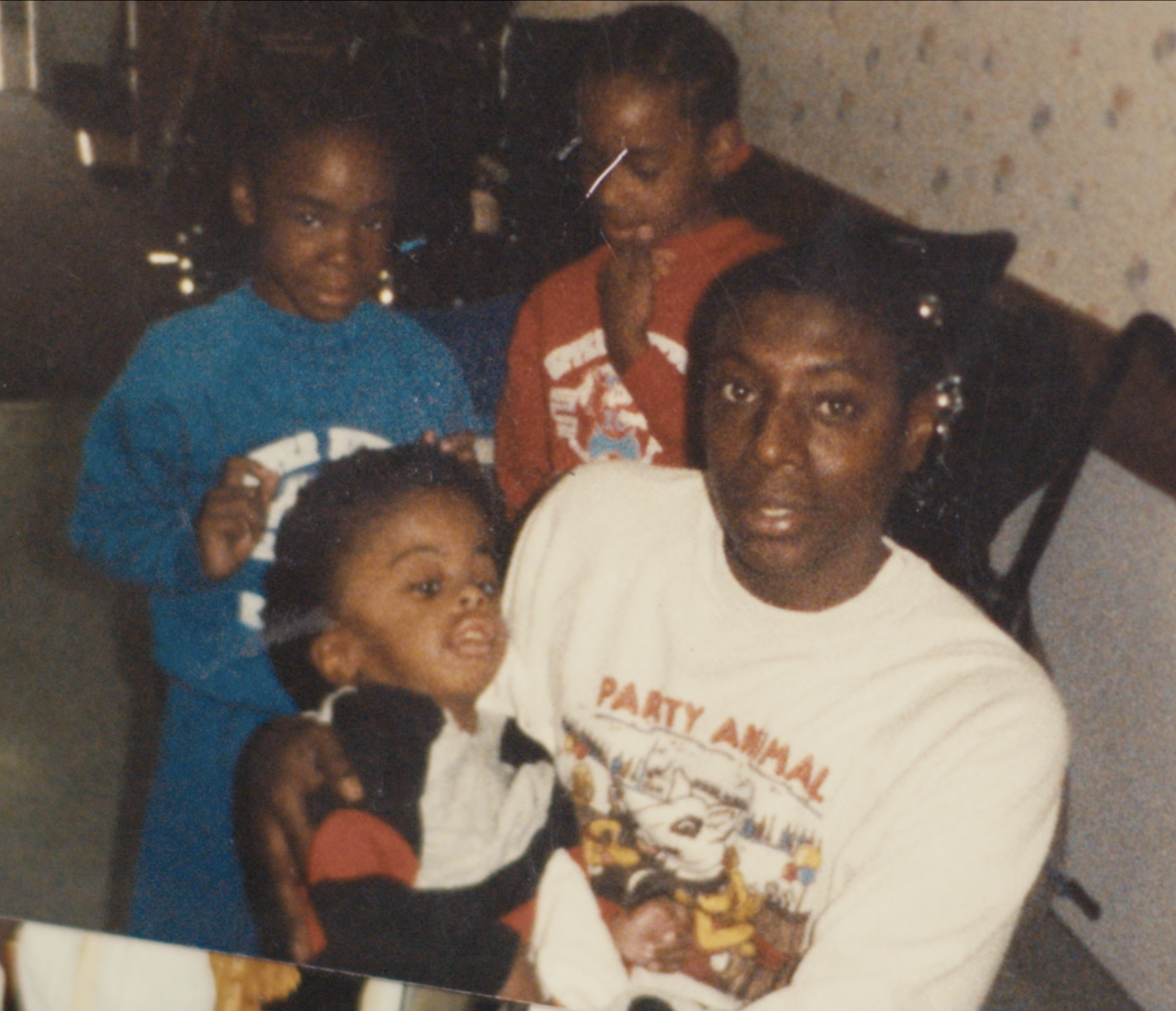
As his daughter Candice and stepson Aubrey got older, Adolphus missed out on much of their lives. He’d buy items for their birthday party, then not show up because he was high. He missed school engagements and graduations while in prison. To Aubrey, it seemed like his stepdad was always in prison in his white inmate uniform or on the street chasing his next high. But despite the absences, he was the guy who did the punishing and grounding, even from prison.
Out on parole violations, Adolphus went to a treatment center for four months only to return to using. Audrey told him she couldn’t go on and refused to see him again. Candice would have nothing to do with her father. He had broken the trust of his loved ones too many times.
The one person Adolphus remained close to was his stepson, Aubrey. When Adolphus was around, Aubrey idolized him for his good looks, charismatic manner, and presence. But the anguish of Adolphus’ constant absence haunted him well into adulthood. He followed his stepfather’s path, using drugs and spending time in prison.

Yet where Aubrey’s journey differed from his stepfather’s is that Adolphus’ very absence and failure as a male role model drove Aubrey to finally quit using heroin so he could be there for his own children. One night in 2016, he chose his family over drugs.
That night, he had a handful of dope he’d already started taking when he realized he was supposed to be at Candice’s home. “I’m not going,” he thought. “I started doing them.” Then he asked himself, “What if they come home and you’re dead? Because you know your son will come running in looking for you.”
He threw his stash in the toilet and flushed it away. “I’m a father before anything,” he vowed.
REVOLVING DOORS

Recovering from a stroke in 2014, 53-year-old Adolphus was diagnosed with COPD, diabetes, and high blood pressure. Three years later, the IOC discovered Adolphus among some of the top users of hospital and ER resources in claims data. His doctor at the time, Paige Patterson, MD, brought him to the IOC’s temporary location (it subsequently moved to West Valley to be more accessible to its patient community). When Adolphus went down to the University Hospital basement with her, he knew all too well what else was on that floor. “Damn,” he thought. “Is this part of the morgue?”


By the summer of 2017 summer, about half the IOC staff had left. The reasons for the exodus were complex. The shift to what Weir would call “a social work clinic with a medical component” was not what some clinic employees had signed up for. Nor were duties like visiting patients at their homes or absorbing the secondhand trauma from intensively listening to their complex stories.
Ryan Morgan’s experience working as a therapist with patients who had complex trauma histories at Hill Air Force Base proved invaluable to the nascent clinic. He underscored for his colleagues how an integrated model of social work could help provide the trauma context necessary to navigate undiagnosed medical issues such as diffuse body pain with no seeming cause.
As the clinic evolved, Weir also learned from the IOC’s social workers how combatting the lack of trust patients historically felt with providers would be fundamental to their success. That could be attributed to several factors: the sterile environment, the strict time limits on provider-patient encounters, or how blatantly many doctors were about a patient being too complicated to care for.
Even so, the IOC’s instability continued. The clinic went through two case managers, three physician assistants, several medical assistants, and multiple social workers. Staff would exchange looks that boiled down to, “Who will be here next week?”

The provider turnover frustrated some patients. As they re-told their story to each new incoming provider, it only reminded them of how providers at other clinics wouldn’t listen to them, bumping them instead to another doctor. Weir knew there was no easy answer to that dilemma. Staff inevitably moved on for career advancement, personal reasons, or burnout. Yet he could see that every time that happened, it was harmful to their patients.
ONE MORE CHANCE

At first, Adolphus didn’t trust the IOC staff, so he told them what he thought they wanted to hear. Morgan knew about addiction through his father’s struggles with alcoholism. That was what took him into therapy. He understood that addiction equaled isolation—where the world narrows down to the quest for the substance you use and everything else (family, shelter, food, employment) becomes an ever-more distant second. The problem for therapists and treatment providers, however, was that often it was hard to see the human being for their addiction.
“How do I know you aren’t out getting high?” Morgan asked Adolphus. “Because I wouldn’t be seeing you,” Adolphus replied. “I wouldn’t be here.”
Adolphus kept his promise. His next appointment was a no-show and he didn’t answer phone calls. Within months, he was back in jail and then in treatment. But at the treatment center’s classes, all Adolphus could think about was the street.

Morgan contacted him to encourage him to graduate from treatment and go to outpatient services. “I don’t want to talk to you guys,” he told Morgan. “You don’t know what you’re talking about.”
The treatment center helped him get a housing voucher, then an apartment in downtown Salt Lake City near the Department of Workforce Services. In mid-2018, Adolphus told his IOC team that he was done with his treatment and felt fine. But Kay McMahon, PA, a recently hired IOC medical provider, was far from convinced.

By the time McMahon started working at the IOC, two medical providers had left. For six months, she was on her own taking care of 75 patients. There were moments when she felt a little frustrated, even struggling with burnout, but her commitment to the clinic and its vision kept her buoyed throughout.
Burnout from taking care of challenging patients was something that Weir had anticipated, constructing a clinic model that was employee-friendly, with flexible hours, group activities, lunches, and trips to build morale.
McMahon worked hard to overcome Adolphus’ initial mistrust because he had already seen two providers at the IOC in a short period. Because he was so sick with COPD and in the midst of substance use recovery—all while talking about being finished with treatment—McMahon was so scared it made her hair stand on end.
Again, Adolphus fell off the IOC’s radar. They kept pushing and checking in on him, only to get radio silence. He spent his rent money on drugs, let people from the street shower and party at his apartment, and soon lost his housing voucher. He reached out to the IOC for help getting his apartment back, but Morgan wanted to have a wider conversation.
“I think we need to get you back into treatment,” Morgan said. “Let's try to figure that out.” But Adolphus wasn’t listening. For a few months, he managed to keep a hotel room going. Adolphus continued showing up in the ER again and again with crack-triggered respiratory failure, though. Morgan told him repeatedly he needed treatment. After that fifth ER visit in November 2018, Adolphus agreed.
Morgan called him. “I got you a bed—the only thing you’ve got to do is show up for it.” Adolphus was at the front door of the treatment center the next day. “This is your third time,” an employee said. “Please make it your last.”
When Morgan visited him, touring the facilities with his case manager, Adolphus thanked him. “I appreciate you helping me get my start again. And I’m not gonna let you down.”
A ROOM WITH A VIEW

Adolphus graduated from the treatment center to a clean and sober living facility in Sandy, but after a few months there felt that wasn’t working for him. He and Morgan fought over his decision to build his own 12-step program.
“We need to keep up with the treatment center’s 12-step program,” Morgan said adamantly. “Have you ever been addicted?” Adolphus asked. Morgan said no but that he had grown up addiction-adjacent with his father. “You have never been in addiction, and you don't know what's going to work for me,” Adolphus insisted. “You need to listen to me.”

Morgan was furious. He had helped Adolphus into treatment when he was dying on the sidewalk, hadn’t he? But then his anger ebbed as he realized Adolphus was right. “If he isn't driving the bus and telling me what was going to work for him, and I’m not listening to him, then nothing I say or do is going to matter,” he thought. He had to let Adolphus put together a program that worked for him.
Adolphus took TRAX from Sandy to downtown Salt Lake City every day to look for a rental apartment. A complex around the back of the Gateway accepted his application for a sixth-floor one-bedroom apartment. That wasn’t his only success that summer. He also reconnected with his family. He and his stepson Aubrey hung out together, finally bonded by family rather than addiction. Adolphus had also become closer to his daughter, Candice. Aubrey asked his mom if he could bring Adolphus to her 2019 Fourth of July barbecue at her Ogden home. She agreed.

It had been 14 years since the former partners had seen each other, and as they sat around on her deck into the evening, he told her he was starting over. “I’m clean. I don’t want to do this no more.”
“That’s good,” she replied. “I’m happy for you.” That night was huge for Aubrey, with his sober stepfather by his side. But for Audrey, she had been there so many times before. Despite Audrey’s evident caution, Adolphus was convinced that she looked at him in a way she hadn’t since 1985. “She sees me again,” he thought. “The real me, the caring person, the guy who puts family first.”

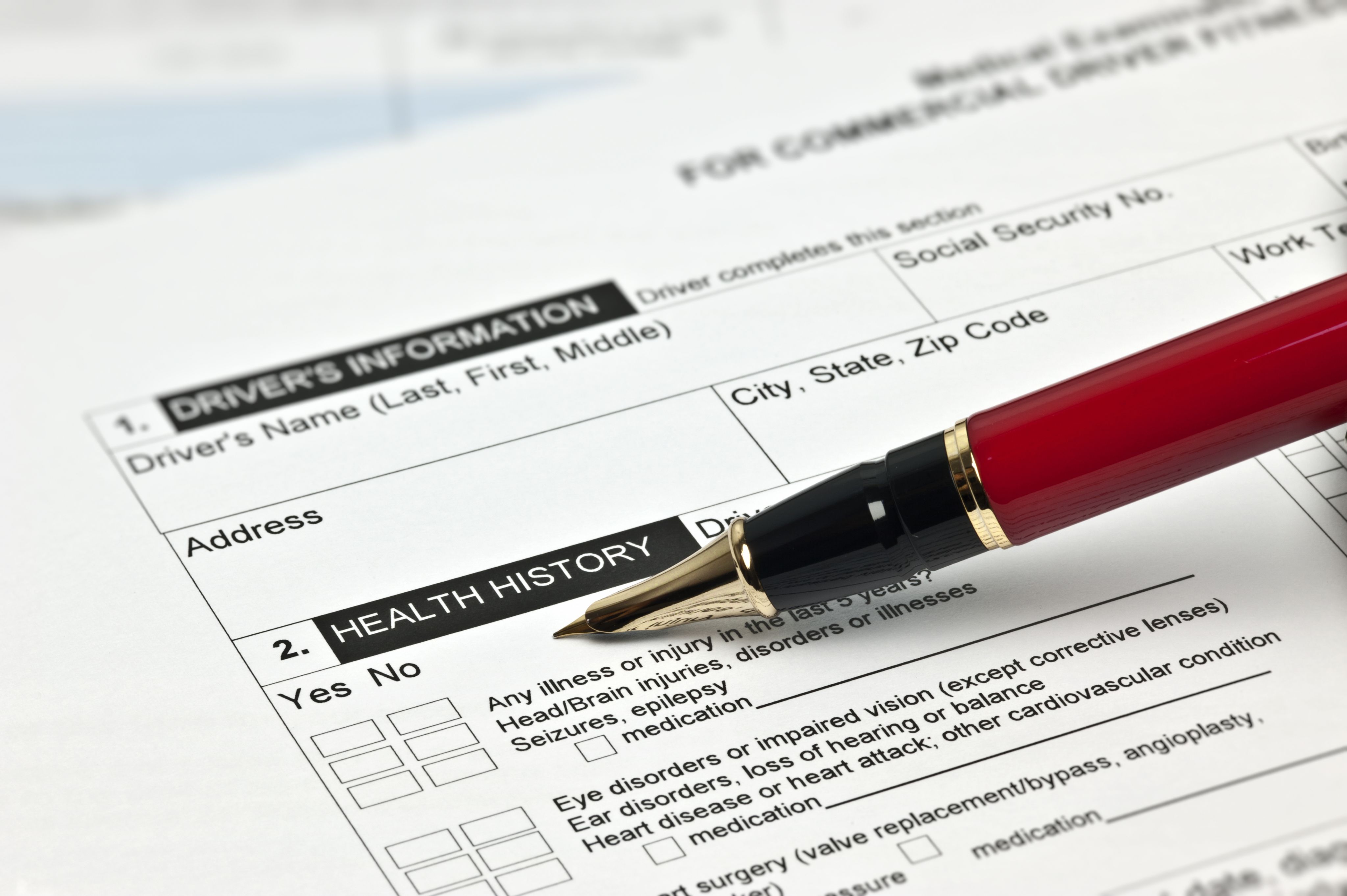
Up until then, Craig Holbrook, the IOC’s office manager, had been getting Adolphus to clinic appointments using Uber. More recently, he had taught Adolphus to request his own pickups on the phone. If he could get his own car, driver’s license, and insurance, Adolphus thought, he could drive to see his grandkids, nephews, and nieces and take them to the park or the arcade.


On September 14, 2019, a nervous Adolphus moved into the Gateway apartment. When he woke up the next morning, he opened the sliding glass door and stepped out on the balcony, looking towards Gateway Mall and the Wasatch Mountains beyond. “Hell yeah,” he thought. “This is mine.”


On September 14, 2019, a nervous Adolphus moved into the Gateway apartment. When he woke up the next morning, he opened the sliding glass door and stepped out on the balcony, looking towards Gateway Mall and the Wasatch Mountains beyond. “Hell yeah,” he thought. “This is mine.”
A CLEAN RECORD
At the same time, the IOC was improving their patients’ lives rather than simply providing medical care. Because the clinic was in a more stable place, Weir knew it would be good timing to bring on new leadership. He would hire his replacement as medical director.
Weir tapped Stacey Bank, MD, a family medicine provider, to pick up the reins. Weir felt that Bank could bring a more nuanced management style, make more incremental changes, and build more depth of talent in the IOC.

Bank started in September 2019—the same month that Adolphus moved into his new apartment. She quickly learned how unique the IOC was. At her old clinic, if a patient didn’t come to an appointment, it was difficult to make follow-up calls. But at the IOC, there was an expectation that since some patients simply didn’t have the physical, mental, or intellectual capacities to navigate the health care system, especially when they most needed help, those follow-up calls to a struggling patient who had fallen off the radar were an essential part of the practice.
Six months after Bank joined, the COVID-19 pandemic began. For eight months, the clinic closed its doors and operated virtually. All the services and meetings to address roadblocks such as missing ID papers with Social Security or a Section 8 voucher with a local housing authority abruptly stopped. Other services such as home visits, outreach when patients fell off the grid, staff accompanying patients with anxiety to their appointments, or doing diabetes education and helping with benefit applications ground to a halt while the clinic operated online only.

For many patients, the clinic and its staff were their only point of contact with anyone else. The clinic was like family, and they missed the structure of regular appointments within a defined physical space. Several patients decompensated behaviorally.
While some of Adolphus’ fellow IOC patients struggled with deteriorating mental health, Adolphus was unphased. He continued his meetings online, exercised, watched The Young and the Restless—his favorite soap opera for 30 years—and, when he saw homeless men on the streets with no one to talk to, tried to offer them comfort, sharing a few words, thoughts, and support. His own response to their plight surprised him. Unless they had money to buy drugs, the old Adolphus wouldn’t have given them a second thought.
He wanted to do more for the addicted, the homeless, and the formerly incarcerated, along with for teens drawn to the lifepath that he had followed. But he feared he could never become a counselor with his lengthy criminal record.

He worked with Michelle Betts, his case manager at the time, to apply to the Board of Pardons for a pardon for his 27 convictions—seven of them felonies, the rest misdemeanors. He and Betts operated like a two-on-two basketball game. She was the point guard, and he was the center. Everything flowed through her, and she guided him to do specific tasks. He completed all the leg work, returning to prisons and jails to retrieve records, including discipline and other paperwork. Together, they turned in the 190-page application.
As Bank learned from and led the IOC team, she came to recognize that one of the clinic’s greatest strengths was the longevity of patient-provider relationships. When one patient refused to acknowledge that a urine analysis was hers, she stood up to stomp out.
“I know you,” Bank pleaded with her. “You know me. Let's just take a breath and we're gonna get through this.” The patient sat down, and they cried together. The patient admitted she had used drugs, and they made a plan to move forward. Those were experiences you only had after being with a patient for a long time, Bank thought.
So how to take these lessons and life-saving achievements and extend them beyond the clinic’s walls—or, as others put it, make it scalable? Bank felt the best answer was pods that replicated the clinic’s model rather than continuing to grow in one location. McMahon hoped a new clinic would open in Ogden to serve high-acuity patients there. But Weir had his sights set on answering the scalability question in another way. He had been working on a parallel project—while the IOC cared for the most extreme or most intensive patients, his new initiative would care for patients with lower acuity problems and provide a less intensive approach, much of it online. This largely virtual structure might make it more scalable, he thought.
THE QUEST FOR LOVE

For Adolphus, his life was stabilized with weekly visits to the clinic for therapy with Morgan’s replacement, Steve Edwards, and check-ups with McMahon. He credited McMahon with helping him manage his diabetes, COPD, and other health care needs while also working with him to keep his health as good as it could be. That allowed him to focus his days on his grandsons, nieces, and nephews, giving them his time, support, and love. If he didn’t know how to be a parent to his own kids, he’d learned how to be there for the next generation. One of the people who had taught him was his stepson, Aubrey.
In his determination to be the best dad he could be, Aubrey gave Adolphus the strength to be the best grandfather. But it was more than that. Adolphus saw his stepson as a better dad but also a better person—more laid-back, more open, more humble.

What Adolphus had long sought was to be wanted—not for dope but for love. “That’s what I want, man, was someone to love me,” he said. “Let me know that, ‘Hey, you’re our guy.’” His 6-year-old grandson Karson was his best friend. Karson always asked him when Adolphus was about to leave after visiting him: “When are you coming back?” “When will I see you again?”
Adolphus and his grandson together watched the short film, “Meet Me Where I Am,” that the IOC and Adolphus produced with University of Utah Health and a team of independent filmmakers in 2022. Karson asked his grandfather about prison, why he went there, and what it was like. Adolphus did his best to answer his questions honestly and frankly.

“I don't want him to see his grandpa running in and out of his life, you know, and not doing the right thing,” Adolphus said. And he didn’t want Karson to go down the same paths he took. “I want him to be one of the best people that he can be in life.”
FROM HURTING
TO HEALING

As much as Adolphus wanted to be a positive influence on the next generation, he, his life story, and the IOC were also impacting a much wider circle than solely the health care world.
One Tuesday afternoon in May 2022, Adolphus waited nervously in the clinic’s reception area as officials from the Department of Corrections, Adult Probation, and Parole, Utah’s government planning and budget office, and U of U Health Plans arrived for a screening of his film and a discussion about some of the issues it raised. In total, close to 30 people filled the room. Adolphus couldn’t help but notice he was the only Black person in the room.
After the movie was shown to applause, Adolphus told the room, at Bank’s prompting, that he had recently certified as a peer support specialist. “I’m ready to help whoever needs it,” he said.

One official called what the film revealed about the IOC’s work with Adolphus and its 125 patients “the holy grail,” taking a trauma-informed approach to care to “treat people like human beings.” Another added, “It’s just a seed planting at this point. But we have to figure out how to capitalize on this beautiful thing you’re doing.”
Some of the conversation focused on cost savings, a theme central to the success of the IOC model. Bank told the room the IOC was saving U of U Health Plans about $2-3 for every $1 they spent on the clinic. One official spoke up emotionally, drawing nods of recognition and approval from law enforcement and correction officers. “Instead of hurting people, we can be healing people,” she said.
A corrections employee argued that the prison needed to rethink re-entry specialists within a social work context. “This is the model here,” he said about the IOC’s work. “We can be part of that.” Adolphus summed up the meeting and its surprising nature in awestruck tones. “I didn’t think I’d ever be in a room like this,” he said.
After the meeting, several people from the criminal justice system wanted to talk to him about possible jobs advising inmates on re-entry or officials on systems change. At home, Adolphus worried that if he did work within the corrections system that his voice might end up being sidelined if he pushed too hard for change. He was determined to keep his focus on a pardon for his convictions for now.
Part of him was also drawn to working with young people. Each time there was a school shooting or mass shooting by a youth, Adolphus was reminded of when he took a gun to school—and how close he had been to using it. “I don’t want to be the bad guy no more. I want to be the good guy. I want them to be good kids. I want them to go to school, to graduate, to have a purpose in life. I never had that purpose.”

Adolphus takes pride in the purpose he sees in his stepson and how Aubrey taught him how to be a father. When Aubrey comes to visit with his 4-year-old son, Adolphus admires how Aubrey cooks for his children and focuses on them. Aubrey has hopes for his life now.
They may not be blood kin, but in every other sense they are related. “I have a father,” Aubrey says, smiling through his tears. Adolphus looks at him. “That’s my son right there.”

TRUST AS CURRENCY
Story by Stephen Dark
Portrait photography by Louis Arévalo
Design by Laurie Robison
Edited and published by Nick McGregor
Film stills from "Meet Me Where I Am"
Additional contributions from
Joe Borgenicht, André Robert Lee, Ross Kaufmann, Robin Honan, Peter Weir, Stacey Bank, Christina Cackler, Kay McMahon, and the entire IOC staff
Special thanks to
Adolphus Nickleberry, Candice Drawn, Aubrey Drawn, and their entire families
