They Emerge Transformed
Burn survivors and those who care for them at University of Utah Health Burn Center share a fundamental truth few others know

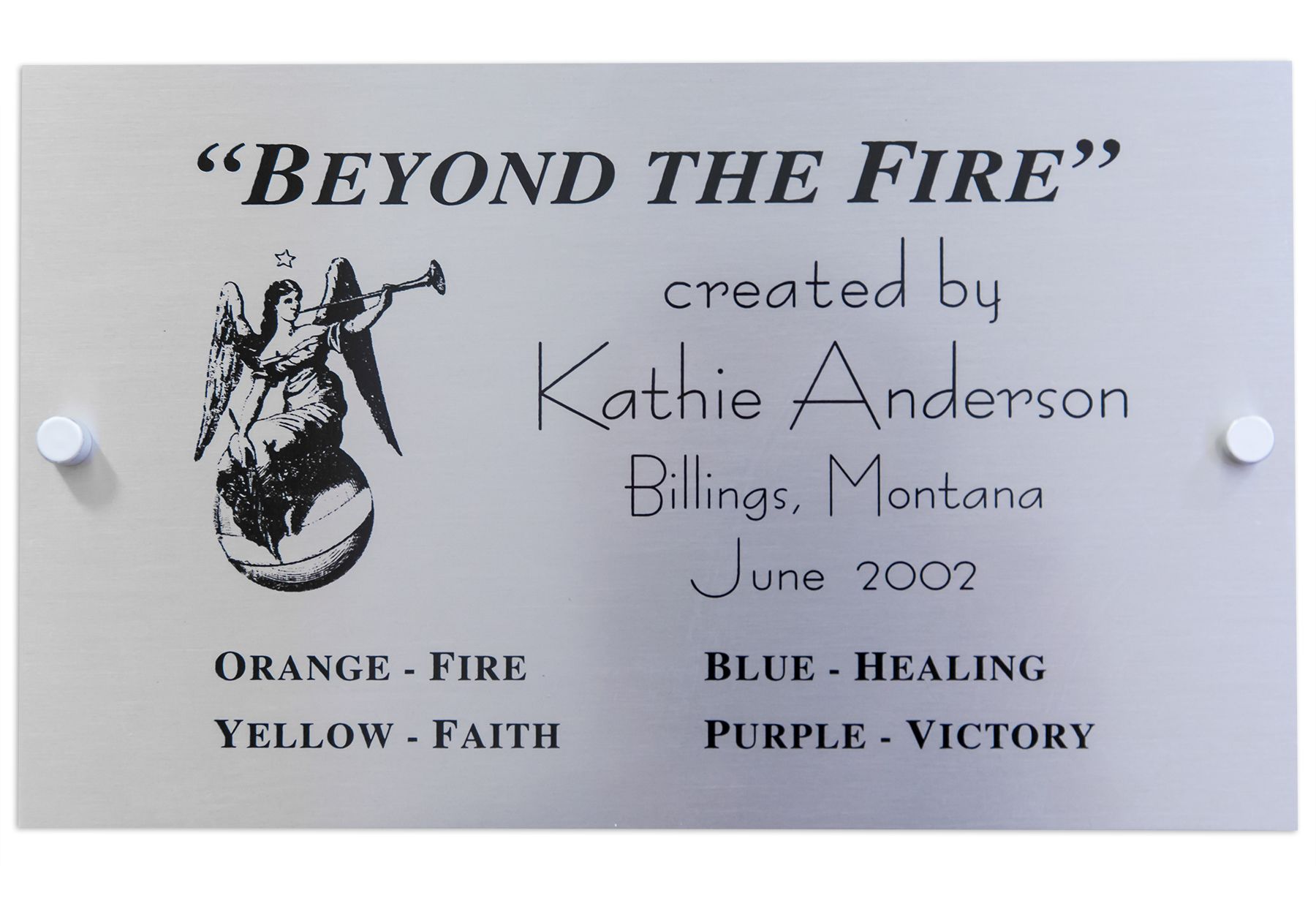
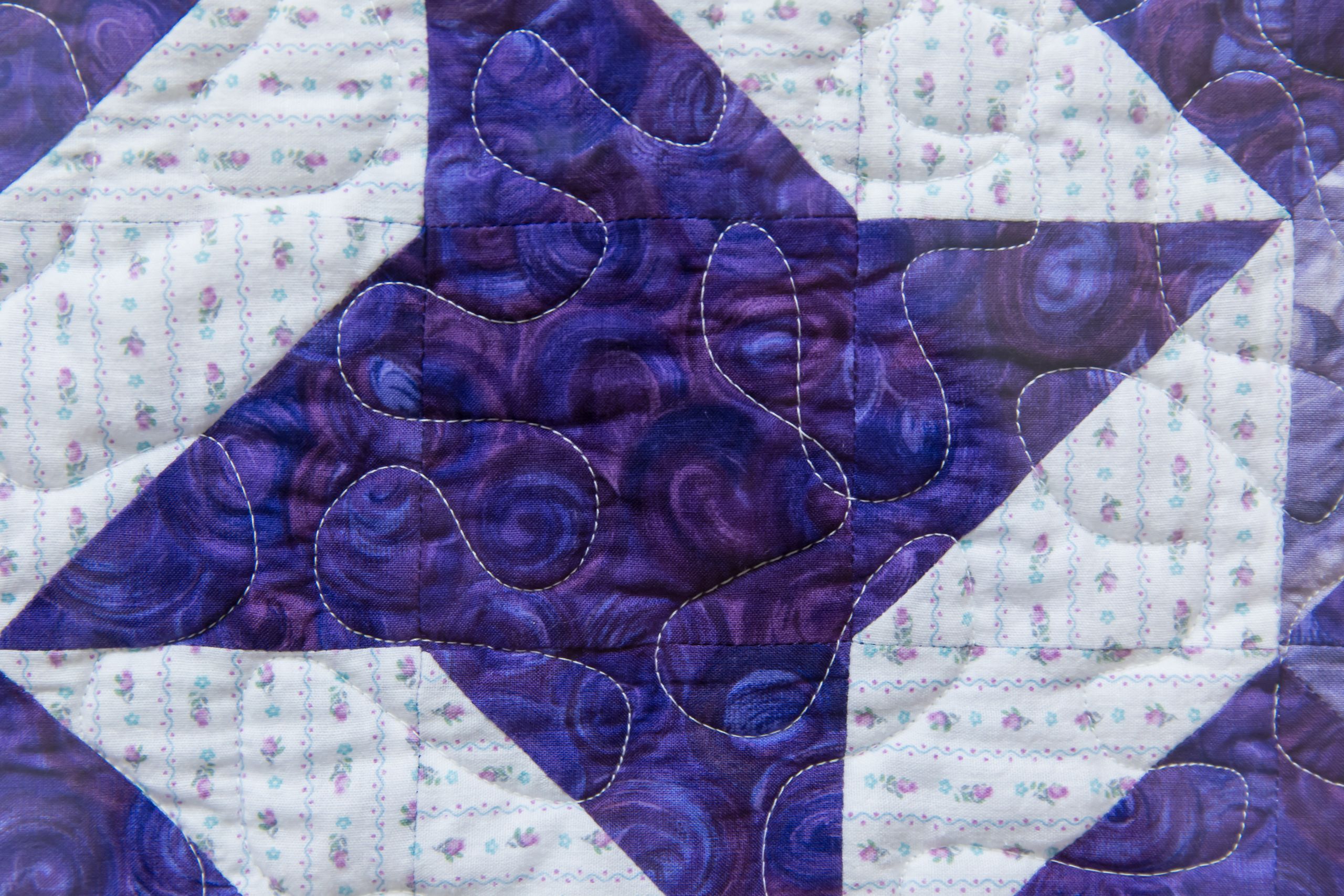
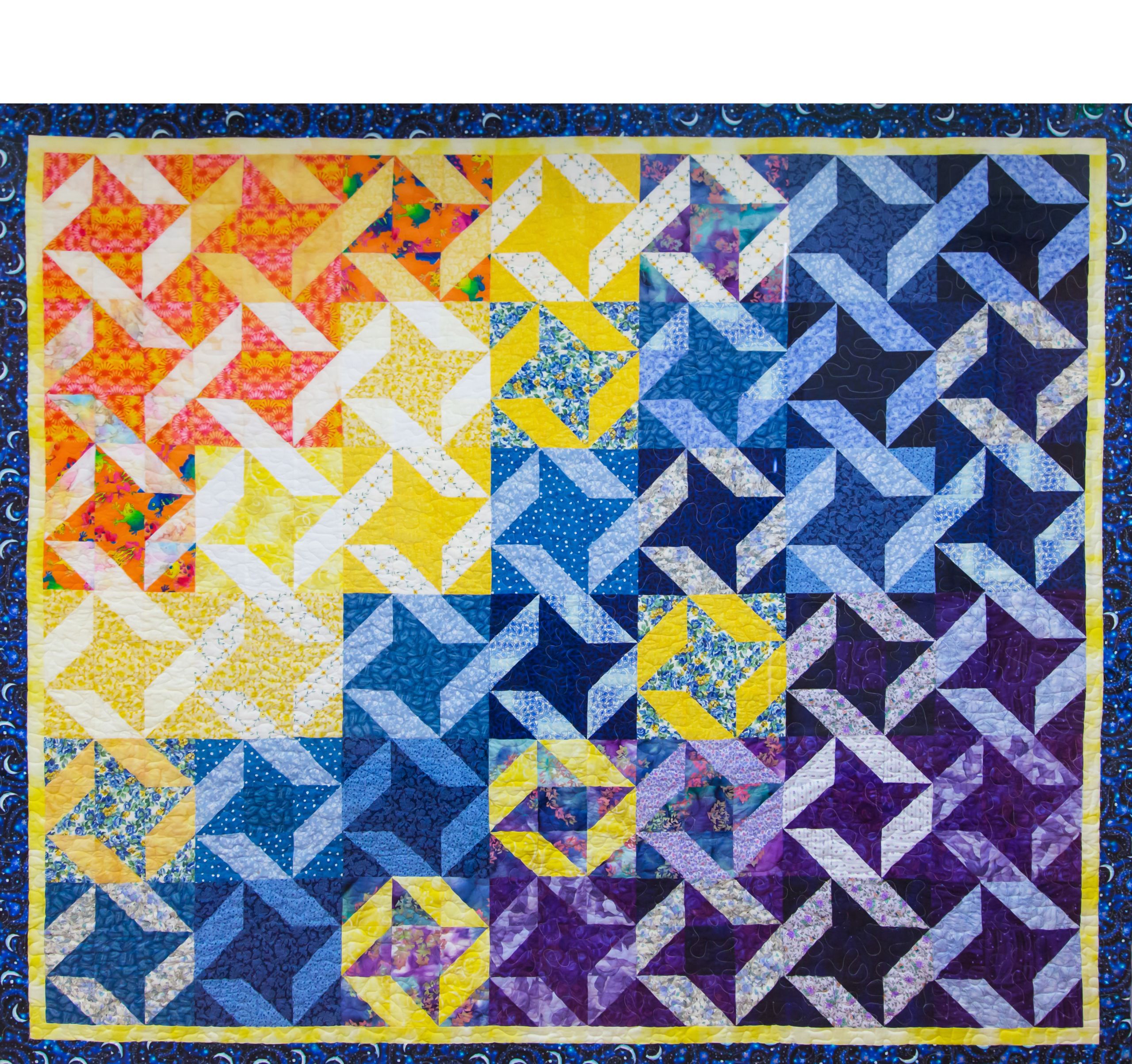
The burn center is tucked away on the fourth floor of University Hospital. Opposite the door to nurse manager Brad Wiggins’ office hangs a framed quilt, titled “Beyond the Fire.” Donated in 2002 by Kathie Anderson, four waves of colors—orange, yellow, blue, and purple—cascade down from top left to bottom right.
According to a plate next to the quilt, orange represents fire, yellow represents faith, blue represents healing, and purple represents victory. The key suggests a narrative of a patient’s journey, from being burned through many months of inpatient treatment at the center, to a new life outside the hospital in a world utterly unfamiliar with all they’ve gone through.

The importance of quilts to the center’s patients extends beyond the artistic rendering of progress from injury to release. Quilts piled up in a closet keep patients warm; if a burn has removed much of their skin—the body’s largest organ—maintaining their body temperature is a constant battle.
The quilts also capture what the center does:
“We are a patchwork quilt made to encompass the patient, to make them feel warm and safe,” one nurse said.
FIRE

Daniel Pavon’s eyes had been sewn shut for four months.
He and three other “rough necks” had been working on a western North Dakota oil rig when a gas pipe split and ignited. On fire, Pavon was blown backwards by the blast, only for his foot to get caught in a hand rail, leaving him hanging upside down on some metal steps.
Oil rig workers put him out with fire extinguishers and helped him off the platform. Paramedics couldn’t find a vein in his blistered body and drilled a hole in his knee to give him morphine. He was airlifted to the nearest burn center in St. Paul, Minnesota, where he learned 77% of his skin was burned.
“Who’s going to feed my family?” he thought.
Doctors sutured his eyes closed to allow his scarred corneas and eyelids to heal. While he was temporarily blinded, he relied on his imagination to conjure up those around him.
When doctors opened one eye, all he could see at first were shapes and blurs. Without telling anyone, Pavon decided to see for himself what damage the fire had done. He went to the physical therapy room and stood before a full-length mirror.
Despite his psychologist’s preparation for coming to terms with his visage, he’d never seen a burn survivor before. He’d had a full skin graft on his face, the skin red, blotchy, and uneven. He’d lost both his ears, parts of his nose and lips, his hair and eyebrows, four fingers, and so much of his skin that he didn’t recognize himself. He drew in a shuddering breath through the scar-tight hole where his lips had been.
“How will my family and friends react?” he wondered.
He was flown to Salt Lake City to continue treatment in the University of Utah Health Burn Center, where he could be closer to his family, especially his wife, Ana, and son, Daniel Jr.
“It was hard for me to accept help,” Pavon said, sitting in the living room of his Loma, Colorado, home, surrounded by acres of sun-ripened corn under a bright blue sky. “I couldn’t even feed myself. I couldn’t even wipe my own eyes. They’re always tearing.”


He and three other “rough necks” had been working on a western North Dakota oil rig when a gas pipe split and ignited. On fire, Pavon was blown backwards by the blast, only for his foot to get caught in a hand rail, leaving him hanging upside down on some metal steps.
Oil rig workers put him out with fire extinguishers and helped him off the platform. Paramedics couldn’t find a vein in his blistered body and drilled a hole in his knee to give him morphine. He was airlifted to the nearest burn center in St. Paul, Minnesota, where he learned 77% of his skin was burned.
“Who’s going to feed my family?” he thought.
Doctors sutured his eyes closed to allow his scarred corneas and eyelids to heal. While he was temporarily blind, he relied on his imagination to conjure up those around him.
When doctors opened one eye, all he could see at first were shapes and blurs. Without telling anyone, Pavon decided to see for himself what damage the fire had done. He went to the physical therapy room and stood before a full-length mirror.
Despite his psychologist’s preparation for coming to terms with his visage, he’d never seen a burn survivor before. He’d had a full skin graft on his face, the skin red, blotchy, and uneven. He’d lost both his ears, parts of his nose and lips, his hair and eyebrows, four fingers, and so much of his skin that he didn’t recognize himself. He drew in a shuddering breath through the scar-tight hole where his lips had been.
“How will my family and friends react?” he wondered.
He was flown to Salt Lake City to continue treatment in the University of Utah Health Burn Center, where he could be closer to his family, especially his wife, Ana, and his son, Daniel Jr.
“It was hard for me to accept help,” Pavon said, sitting in the living room of his Loma, Colorado, home, surrounded by acres of sun-ripened corn under a bright blue sky. “I couldn’t even feed myself. I couldn’t even wipe my own eyes. They’re always tearing.”


THE GUARDIANS
From its humble beginnings in 1976, the University of Utah Health Burn Center has become one of the 73 “verified” top centers in the world—a title of independently audited excellence it has held since 1992. It’s seasoned in the consequences of human behavior, which run the gamut from acts of selflessness, bravery, and sacrifice to unthinkable behavior rooted in selfishness, indifference, and cruelty.
Double doors swing open to a unit where most staff are in pale blue scrubs, underscoring the egalitarian nature of burn care, where everyone from the most junior health care assistant (HCA) on up is expected to advocate for patients in their care. Patients’ rooms, most with their doors closed and blinds lowered, run along three sides of a rectangular corridor. Along with nurses’ stations and what’s known as “the fish bowl”—where staff meet to review cases for training and sometimes tears after a patient’s death—in one corner stands the doors to the operating room.
In this mini-hospital within a hospital, burn care is rendered holistically, with support from a multidisciplinary team of physicians, nurses, social workers, a pharmacist, a psychologist, a child-life specialist, and respiratory, physical, and occupational therapists, among many others.
With approximately 400 patients annually, the injuries the center treats range from flame and chemical scalds to electrical, frostbite, and soft tissue injuries such as flesh-eating bacteria. Burns are excruciatingly painful, exposed nerve endings enduring bacteria-cleansing scrubbing during wound care. Despite the team’s tireless work, around 25 patients die each year.
Many of the center’s 102 employees view their work not only as vocational but also sacred. “This is a place where patients can be safe from harm from other human beings and physical phenomena,” said Stephen Morris, MD, a surgeon at the center for 30 years who stepped down as medical director at the end of 2019.
“We are there,” Morris said, “standing guard to protect people who can’t protect themselves.”
A LOVE SUPREME
“It’s never just a burn,” is oft-repeated by staff, particularly regarding socially and economically marginalized patients who often make up the bulk of those on their roster. “Trauma is a disease of the poor and burns are traumatic injuries,” said social worker Gretchen James. For some marginalized community members, poverty, untreated mental health and substance abuse issues, lack of resources and support systems are among the factors that can lead to traumatic injuries. “There’s usually a reason people end up with a burn,” James said. “It’s rare that it’s just an accident.”
That includes children, who make up a third of the burn center’s patients—90% of them under the age of 3 and around 20% of them abuse survivors. A scalded or burned baby energizes the center quite like no other patient, staff said. “Children are naturally attracted to risky behaviors without understanding the full consequence,” Wiggins said.
Burns demand a culture of care defined primarily by continued treatment that can stretch through months to even close to a year. Surgeries, skin grafts, and physical therapy all help prepare patients for return to the outside world. Burn surgeons and, even more so, the center’s nurses marinate in a patient’s day-to-day life, struggles, and pain. The center at times displays the gallows humor, exhaustion, and intense cohesiveness that marked Wiggins’ grandmother’s time as a World War II MASH unit nurse in France—and the Alan Alda TV show “M*A*S*H” the nurse manager watched avidly as a child.
When a new patient arrives, said Irma Fleming, MD, the newest surgeon to join the center, it’s as if they’re the bride or groom at a shotgun wedding. “We just got engaged when you all hit the door,” she said. “The operating room will be our wedding.” Ad-hoc families are formed by the patient, the relatives, and the caregivers that resonate with the emotional subtexts and occasional dysfunction of any family. There’ll be arguments and tears, reclamations and mutual moments of understanding. “You might think you can divorce us, but there’s no divorce,” Fleming said with a smile.
Patients came up with the term “cocoon of love” for a place they’d invariably not want to leave for the harsh world’s stares that often await them. Yet, at the same time, said Kristen Quinn, who runs the 20-year-old, late-summer burn camp in the Wasatch Front mountains, “cocoon” reflects the process of transformational growth they go through. “When they leave, they are different,” she said, their lives reframed not only by burn treatment but also by the deeply complex and intimate relationships between patients and those who care for them. “They emerge transformed.”
And when it comes time to go home to their biological family, some feel scared. “They curse us, throw things at us, and say, ‘We’ll still come back—I’m going to miss my bubble of love,’” Fleming said. “That’s the part that makes it OK. They know it was done out of love.”
FAITH

“I was born with the perfect skin,” Joseph Martinez, a Ute Tribe member, said.
“I could stand out in the sun all day and never have to worry about skin cancer.” That ended in July 2008, when Martinez was showered with molten tar after a kinked-up hose exploded while he was working for an asphalt maintenance crew in Parley’s Canyon above Salt Lake City. His boss’ father took him to a nearby hospital, but no one knew how to remove the tar—until a custodian suggested Neosporin, a chemical that separates oil from tar.
“Out of all these doctors and nurses, it was a janitor that saved me,” Martinez said, shaking his head. “Loved that one.”
He was transferred to the University of Utah Health Burn Center; despite the pain he was in, he refused Lortab. His culture views the body as a sacred gift of the creator and drugs as a poison. He survived four weeks of agony before finally accepting a painkiller.
It wasn’t only physical pain that haunted him, but also feelings of isolation. He had no other native patients to talk to. No one to share the often-brutal nature of what his care involved or the anger at how his employer had treated him in the wake of the accident. “I didn’t have anybody I could really talk to,” he said. He had nightmares of someone grabbing his long hair, which had once hung all the way down his back, and pouring tar on his face.
Although Martinez had no one else at the center who understood his cultural needs and concerns, Native Americans are often on the center’s patient roster. Martinez argued that their presence stemmed from both individual responsibility and poverty, depression on the reservation and “just the hardship of life.” He understood all too well the center’s mantra of “It’s never just a burn.” Living conditions imposed by poverty in Utah and neighboring states, he said, were often significant factors in why and how many of society’s most vulnerable and marginalized come to be in their care.
Martinez joined U of U Health’s Survivors Offering Assistance in Recovery (SOAR) program to advocate for and support native families. SOAR trains survivors like Martinez and Pavon so they can aid others who have experienced similar injuries. For all the pain Martinez suffered, his burn taught him he could get through anything.
“I learned you really can’t say ‘No’ to life because it’s so short,” he said. “Before I got burned, all I did was work and go home. I never said ‘Yes’ to life. After being burned, I never said ‘No.’”
STAND AND DELIVER
In 1976, when the burn center opened its doors, burn care was viewed by most in the medical profession as the ugly stepchild of medicine—a position it still holds. “The wounds were very messy, hard to care for, very labor intensive, and there was a significant mortality rate,” recalled Jeffrey Saffle, MD, who was the center’s medical director for 30 years.

Glenn Warden, MD, started the center, after completing a fellowship at the Brooke Army Medical Center in Texas. Warden taught Saffle, “You were always on call, always available for patients,” Saffle said. “The team was much more closely knit than other services.” Warden hired Melva Kravitz as nurse manager from another groundbreaking burn center, the Parkland Burn Center in Dallas.
A nurse manager’s position is “very much an advocate role for nurses in burn treatment,” Saffle said. “The care is so intensive, so hands-on at the bedside, it’s harder for them to detach themselves. They become tremendously invested in patients. It’s so satisfying to see them get well; it’s devastating when they don’t.”
Pharmacist Ann Marie Prazak agrees. The fundamental crisis points for many staffers at the center are often “those really tough cases where we’ve worked so hard to help someone survive and they didn’t,” she said. She recalled 15-year-old Bailey Hoaldridge, who was badly burned in an ATV accident and displayed a bravery that touched everyone on the unit. “Her death was hard on all of us."
Saffle took over from Warden as medical director in 1982, hiring a resident, Stephen Morris, as attending in 1988. That began a period of hires of people who inherited and still embody the Warden-Saffle culture.
Nurse manager Wiggins, wound care manager Bret King, psychosocial burn program coordinator Kristen Quinn, and outreach education and disaster coordinator Annette Newman all joined within 12 months of Morris—and are all now 30-year veterans of the burn center.
“Dr. Saffle was God,” Newman said. “We wanted to be perfect for him; we wanted to take care of his patients in a way that he would be proud.”
WORSE THAN DEATH
A burn patient’s prognosis can prove unpredictable. A powerful, resilient-appearing patient may need so much help to get back on their feet, while an unassuming, unheralded individual “will stand and deliver like you can’t believe,” Morris said. Age, health, social standing—nothing can predict what Morris called “the magnificence of some patients in terms of how they rise to meet the challenge.”
In James’ first year as a social worker on the unit, she learned she needed more than a thick skin to work there. “I feel like I had to go through this weird initiation,” she told Wiggins. “I learned about human cruelty and suffering.”
There were worse things than death, she found out— things that happen that people don’t always want to survive.
Sometimes families cling to a loved one and demand the center keep them alive, even though the staff are keenly aware the burn will likely kill the patient. Such cases led to a shift, installing a protocol “trigger” to bring in the palliative care team early rather than late in patient care, said Giavonni Lewis, MD, recently appointed as the center’s new medical director.
Lewis joined the team the day of Saffle’s retirement party, staff mourning the passing of an era. “It was the end of all many of us had known,” Newman said.

Three generations of burn center leadership gathered for the retirement party of Dr. Saffle (center). To Saffle’s left, his successor, Dr. Stephen Morris, and to his right, the current center director, Dr. Giavonni Lewis.
Three generations of burn center leadership gathered for the retirement party of Dr. Saffle (center). To Saffle’s left, his successor, Dr. Stephen Morris, and to his right, the current center director, Dr. Giavonni Lewis.

Staff mourning the passing of an era with Dr. Saffle’s departure.
Staff mourning the passing of an era with Dr. Saffle’s departure.
HEALING

Deshca Demoss was a model as a young child.

Now 11 years old, she entered online pageant photo competitions with the help of her aunt, Savanna Wood. They’d get different boutiques to send her outfits and she’d dress up for a specific theme, such as the princess and the pea. They’d send in her pictures and judges voted on the winner. Deshca won over 15 crowns.
She had had a hard childhood growing up in Blackfoot, Idaho, even before the burn, said her mother, Danielle Wood. She developed a bubbly personality that kept others at bay. “She doesn’t like to let people in,” Danielle Wood said. “She figures if she’s louder than them, she won’t let them in.”
Deshca was 7 years old when she was badly burned in her family’s home. She’d started baking birthday cakes when she was 5, and the day before her brother’s birthday, she asked her grandmother if she could bake a cake.
“It happened after she made the cake,” Danielle Wood said. “She was supposed to be getting ready for bed and she was playing with a lighter. My mom heard the scream and came running out of her bedroom.”
When Danielle Wood got to the Pocatello hospital, shortly before her daughter was transferred to the University of Utah Health Burn Center, a nurse told her to brace herself. She went into Deshca’s room. “All I see is my little girl with blisters across her face and arms and everywhere.”
NO PAIN, NO GAIN
Pain is fundamental to burns—both the actual burn and its treatment. Training for burn surgeons and nurses includes “learning how to shape and mold the pain we’re putting people through,” Fleming said. “As a surgeon, I’ve accepted that I’m going to hurt you to heal you.”
The team has to identify the patient’s limits and how far he or she wants to go. A patient who allows Fleming to do everything she could makes her a better surgeon for the next person.
Wound care is a scheduled part of a patient’s day in a room distinguished by stainless steel doors. Wound care nurses transfer patients to a stainless steel table that, much like the doors, makes it simpler to clean. On the table, they soak patients’ bandages in an effort to make them easier to remove.
Along with removing dressings, nurses and HCAs scrub wounds with washcloths to remove bacteria. “I realized I wasn’t doing anyone a favor being a weenie on their wounds,” said HCA Warren Bailey. “It’s better now than later to increase discomfort.”

In wound care, the stainless steel table provides both ease of cleaning and access to patients for staff charged with scrubbing painful wounds of bacteria.
In wound care, the stainless steel table provides both ease of cleaning and access to patients for staff charged with scrubbing painful wounds of bacteria.
Over two decades, Bret King, the wound care manager, has become an adept student of the nature of pain and the many ways individuals respond to it, including those inflicting it in the name of medicine. The key to effective wound care is getting to know patients’ personalities, he said. This allowed him to build trust as he talked patients through the process. “They know it’s going to be painful; they let you do it anyway. And afterwards, they thank you for doing it.”
Health care assistants and nurses also seek to establish trust with patients over the time they get to know them. Bailey learned that small gestures were so impactful for patients—washing and braiding their hair, cleaning and painting fingernails for women, scrubbing, lotioning, and massaging feet, cleaning behind ears or belly buttons. “They don’t have hands to do it,” he said. “If you try hard to do it, that means a lot.”
Nurses teach patients’ relatives how to perform wound care, a task that made the first four months of Deshca’s stay at the center emotionally and physically draining for her mother and aunt.
They’d play Taylor Swift songs and sing along with Deshca while putting on gowns and gloves and learning from staff how to cut off bandages and peel off compression garments, all while trying to find a way to let the little girl have more control.
“Taking the bandages off and cleaning the wounds—they were nightmares,” Danielle Wood said. “Bandages stick to raw skin and there’s no easy way to get them off. She would fight, kick, scratch, and scream. You definitely need earplugs when you do a dressing. She could wake the dead.”
Pavon also struggled with wound care. But once he understood it was in his interest to go through it, his wife Ana said, he became an active participant in his own care. Patients can choose when to have wound care. Pavon chose after breakfast, getting the pain over with rather than it hanging ominously over his day. “I realized if you don’t do your best, you’re going to stay there longer,” Pavon said.
WHAT WE SEE FIRST
“Skin grafting is a temporization of the wound,” Lewis said. “It closes it but it doesn’t provide the same things they had before the skin was burned.” The burn center, Fleming said in the white-tiled operating room, takes care of “wounds that nobody else wants to deal with.” Necrotizing wounds, infected wounds, burns, skin diseases (people sloughing off all their skin due to a dermatological reaction). “I enjoy getting people through the darkest times of their life,” Fleming said. “It gives me fulfillment to know they are not just out in the world trying to figure it out for themselves.”
After grafting comes “the hardest part,” Lewis said. “Getting people to go through the pain of the process of stretching and moving. That’s a new part of their life. They can’t just jump up and go and do life like they did before.”
The surgeons look for the graft to slowly display color, an indication of healing and attachment to the wound surface. “When I put it on, it’s pale,” Lewis said. “I look at it three days later, it’s pink. It has life.” Infection, immune system depression, or sometimes-unknown reasons can also lead to it not taking.
The physical therapy gym is next door to the OR. It’s not unusual to hear screams coming from there— sometimes bad ones, Bailey said. Pavon stretched out skin grafts that, if he didn’t work them on a daily basis, would shrink. At night, he put tubes into his mouth to stretch out his lip skin grafts. “He’s a heroic patient,” Bailey said. “The work he put in to get his body working, I don’t think most people can do it.”
On Thursdays, Deshca, her arms held up by splints so her underarms could heal, would make her trip with social worker James down four flights of stairs to the cafeteria, which had giant Rice Krispie treats that day of the week. “Make way,” she’d call out, a force of nature stopping passage up and down the stairs as she descended.
“Deshca grew as a person and made friends with other burn survivors in the center,” Savanna Wood said. She would tell injured, struggling adults to buck up. Bandaged from the waist up, her arms in casts, she would tell them, “Look at me, I’m doing good.”
Part of coming to terms with injuries is dealing with the reactions of others. “Our skin is our identifying feature,” Fleming said. “It’s the first thing people see and make assumptions about.”
Patients have to overcome the fears and miscomprehension of others to their burn and facial scars. “And a lot of them get depressed initially because people’s stares tell them they don’t fit into the world anymore,” Fleming said.
What was painful for Pavon was those not inclined to restrain their curiosity. He would go down from the burn center to the first floor’s Starbucks and everyone would stare at him, he said. “That’s not a good feeling.”
One woman said, “So you got burned, heh?”
Released from the hospital, Deshca faced more surgeries and daily stretching, particularly for her underarms, which would tear. There was the daily battle of getting her to wear her “skins”—compression garments made of spandex to keep the skin graft down and reduce scarring.
“It took three years for those wounds to fully close,” her mother said. Each grade, surgeries and recovery kept her out of school for months at a time, putting her behind academically.

Deshca Demoss (top right) with her mother Danielle Wood and Deshca’s siblings celebrating New Year's Eve 2018 in their home. (Courtesy Danielle Wood)
Deshca Demoss (top right) with her mother Danielle Wood and Deshca’s siblings celebrating New Year's Eve 2018 in their home. (Courtesy Danielle Wood)
Like Pavon, some people would unabashedly ask what happened to her. The burn unit taught her phrases before she left.
“My name is Deshca. I’m a burn survivor. Good to meet you.”
VICTORY
Try to understand what victory means to burn survivors and it boils down to living the life they want to live.
Pavon’s passion is quarter horses. That’s what he grew up with in Chihuahua, Mexico, as a child. “They’re like big dogs,” he said. “I love them so much. They don’t talk or bark. You can see in their eyes; that’s the way they speak to me.” He sees his horses every day—it’s a 10-minute drive to the stables—and they are his pride and happiness. “Seeing the little babies grow up and turn into these fast horses, it’s not like a business—it’s something I enjoy.”
One was named Casi Guapo, which means “almost handsome,” something he and a friend were called when they got dressed up to go out one night in Mexico years before the accident. “You guys are not guapo, you’re casi guapo,” someone said.
In early 2018, Casi Guapo won Pavon’s first race. “My heart was in my mouth,” he said. “It was coming out.” Everybody wanted to talk to him, but he just wanted to be alone.
Loved ones of burn survivors have their own journeys. Pavon’s wife Ana has struggled to figure out what to do with her life, she said. Before the accident, she had wanted to be a medical translator and interpreter, but now she’s done with hospitals. “I’ve been supporting Daniel so long, I don’t know what I want to do with myself.”
She found it “super lonely” having to deal with news people, charities, and lawyers in the wake of the oil rig explosion. “Everybody wanted to know things.” Her spouse, the person she’d run to with ideas, was intubated in a burn center. “I didn’t have anyone to run my decisions by. I had to trust what I was doing was what he wanted. And it was.”
In the evening Colorado air, smoky from California’s forest fires, Pavon said he’s so comfortable in his own skin, “I don’t realize sometimes that I’m burned. People who know me, they don’t care about this,” he added, gesturing at the wounds.
In the almost 10 years since Martinez suffered his molten-tar burns, he got divorced and married a woman who lives in Mexico. He runs his hand appreciatively over his forearm. “My skin grafts look so beautiful,” he murmured. The center wasn’t sure why they came out so well, he said. “I eat a lot of wild game: buffalo, elk, and deer. Not steroids—just sagebrush.”

At Disneyland, Martinez shows his wife Ruby the sights in January 2020.
At Disneyland, Martinez shows his wife Ruby the sights in January 2020.
He still works with SOAR to support Native American patients, and he’s on-call for tribal members who are close to death and wish to have a “smudging”—the ritual burning of herbs for a cleansing or blessing—performed in their room.
Deshca lines up for yet another turn on the diving board, her arms crossed over her slight chest, trembling even though the late-summer sun is still high in the sky. She shouts out to Caroline Updike, her favorite camp counselor and the nurse she was closest to in the burn center: “Caroline, watch me!” She runs to the end of the board, grabs her nose, and flies up above the crystal-blue water, executing a perfect tummy-tuck dive bomb into its depths. Then she determinedly doggy-paddles to the side, climbs out, and runs to the back of the line to wait her turn again.
Camp Nah Nah Mah is at first blush the classic American summer camp. It’s like stepping back 50 years, the surrounding trees and mountains of Millcreek Canyon ringing with the joyful screaming of children and adults competing to be heard in the pool.
This burn camp dates back to 1993, when staff took a dozen or so former child patients on a six-day river rafting trip. Wiggins took over its running after the second camp.
“I fell in love with the idea that you can put someone back together and have them learn to be a survivor and not a victim,” Wiggins says.
This afternoon in August 2019 marks Deshca’s third burn camp. She spends some of that afternoon showing a visitor around the shop where campers can spend their hard-earned “burn bucks” on hats, T-shirts, and burn camp stickers. If the place she loves to be most is in the pool, it’s the camaraderie and sense of being surrounded by people like her that makes it feel truly magical.
“At burn camp, I get to meet other burned people like me,” Deshca says. “And I have fun.”
The prior two years she attended, she was unable to use the pool as her young body continued to heal. She also had to do physical therapy twice a day. “She turned something sad into a positive and bought every one of her cabin-mates and her counselors with her burn bucks a little present and put it on their pillow,” says Updike, who has since moved to Arizona. Updike struggles to hold back her tears as she hugs Deshca in gratitude.

One of the challenges at burn camp is a climbing wall. It scared Deshca at first, but after she overcomes her fear, staff can’t get her off it, anointing her queen of the wall.
“I rocked it,” Deshca says impishly. “Get it?” Running off to climb the wall again, she shouts over her shoulder, “Got to maintain my queen status.”
Deshca has also started pursuing activities she once loved. In summer 2018, she did her first pageant photo shoot since the accident. A first crush or a snub that would upset other 11-year-olds she now brushes off. “She knows that life can get a lot harder,” her mother says.


THE BEST ME
The camp’s children stay in a series of cabins. Deshca pushes through the hanging gold curtain of the Charles G. Plummer cabin into a cool interior lined with bunk beds. Costumes tumble out of a box and sparkle has been liberally distributed around the cabin.
“Looks like a unicorn threw up in here,” Updike says, laughing.
For the final night, each cabin prepares a skit for the post-dinner show. Updike explains her idea. “What defines beauty?” she asks. “Not the world’s definition.”
The skit features some of the girls partying and the others wanting to go but feeling wary of being judged. Each girl has to come up with a line expressing their feelings.
“I’m so scared to go,” Deshca says. “What if we’re made fun of?”
“This is coming from your heart and I know that you guys deal with this in your everyday life,” Updike says. “Are people mean to you?”
“Yes,” comes back a full-throated chorus.
“I love all the strength, ladies,” Updike says.
The skit climaxes with a song Updike called “The BEST Me,” which draws its inspiration from "This Is Me" from the movie The Greatest Showman, albeit with a few changes. When they get to the chorus, their voices resoundingly fill the cabin:
Updike’s eyes shine with tears.
“I’ve been burned,” she repeats. “You are not your burn. You are so much more than your burn scar.”
In the fading evening light filtered through a grove of fir trees, Deshca ponders for a moment the question of what she wants to tell the world. Then she tosses her hair back, looks up, and pronounces her verdict, her words echoing back through the close to 50 years of burn center patients finding a place of hope and transformation at the worst moment of their lives.
“I’m beautiful,” she says.
In every face in this 2019 portrait of the burn center’s staff can be found the commitment, resilience, and support burn survivors come to depend on during their long journey to victory.

“They Emerge Transformed”
Story and concept by Stephen Dark
Design by:
Jessica Cagle
Photography by:
Charlie Ehlert
Steven Vargo (portraits of Joseph Martinez)
Savanna Wood (main portrait of Deshca Demoss)
Production support by:
Mitch Sears
Editing by:
Kathy Wilets, Nick McGregor, and Nafisa Masud
Thank you to the staff of University of Utah Health Burn Center for their time, patience, and contributions to this story.

