PIONEERING
THE FUTURE
Stories of Discovery & Innovation
at University of Utah Health
Developing Better Targeted Cancer Therapies
March 2, 2022
With deepening knowledge of the ways in which tumors grow and spread, treatment for many cancers is moving beyond traditional, toxic chemotherapies to more targeted approaches. New treatments currently being evaluated in clinical trials build on findings from Huntsman Cancer Institute labs – and more are on the way. Our scientists are digging deeply into the ways in which cancer cells circumvent the usual limits on cell growth and figuring out how they evade the immune cells that have the potential to keep them in check. They are sifting through data to find distinctions among cancers that once seemed the same, and finding vulnerabilities that different cancers share. Though their approaches are varied, these researchers have a common goal: improving quality of life and extending survival for patients with cancer.
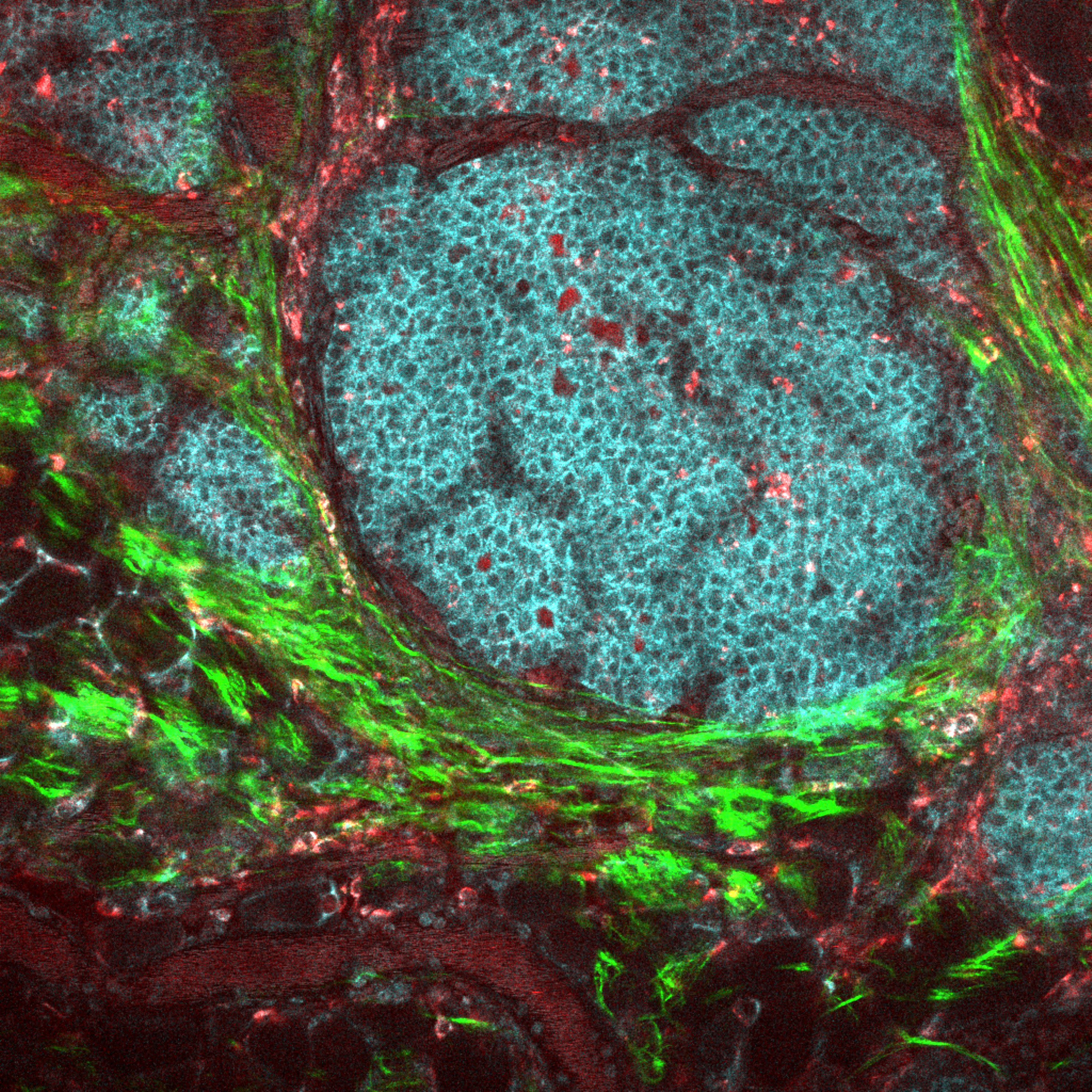
Gliomas are a common and deadly form of brain cancer. A subgroup of these tumors carry mutations in either of two genes that encode metabolic enzymes called isocitrate dehydrogenases (IDH). These shared features might point researchers toward potential targets for treating the disease–but first, researchers need a deeper understanding of how changes to IDH contribute to gliomas’ growth and progression.
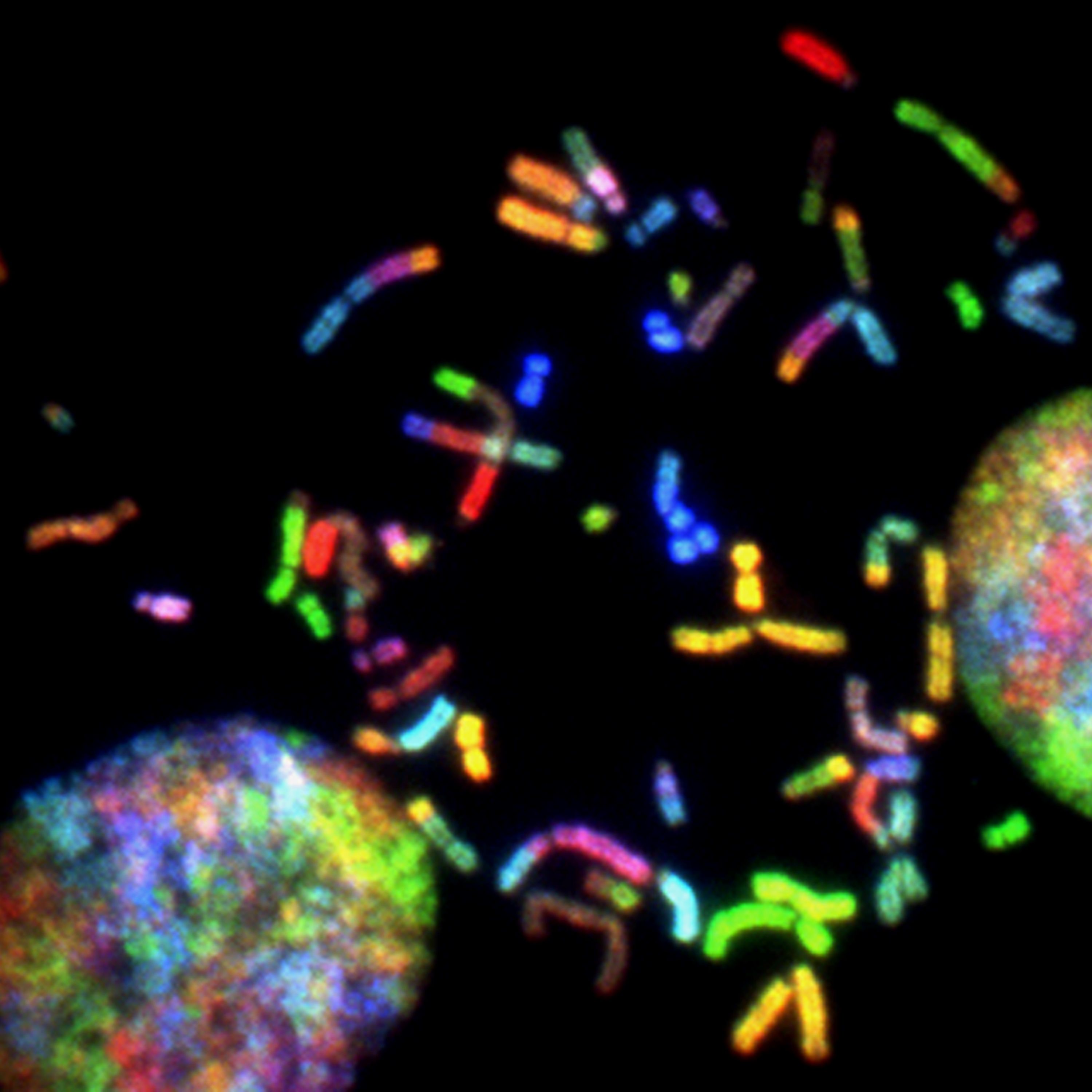
IDH mutations do not cause cancer on their own. However, HCI investigators Sheri Holmen, PhD, Howard Colman, MD, PhD, and colleagues have found that in the presence of certain other cancer-promoting mutations, IDH mutations reliably trigger the development of gliomas in mice. The mouse tumors share key features with patient gliomas, and have expanded researchers’ ability to study the biology of the disease and explore potential treatments. HCI scientists have also demonstrated that not all gliomas with IDH mutations are alike. For example, Howard Colman, MD, PhD, and colleagues have shown that those with widespread DNA alterations tend to grow the fastest. Their findings helped inform updated guidelines issued by the World Health Organization in 2016 for classifying gliomas and other cancers of the central nervous system, which will enable more precise diagnoses for patients.
Researchers have struggled to develop new treatments for pancreatic cancer, an aggressive disease that often kills patients within a year of their diagnosis. Two signaling pathways—one promoting cell growth and the other enabling cancer cells to recycle their own components—are known to help drive the disease. But while drugs are available to block both of these pathways, none have proven effective against pancreatic cancer.
Through laboratory experiments and clinical experience, HCI researchers Conan Kinsey, MD, PhD, and Martin McMahon, PhD, have discovered that the key may be targeting both pathways at once. They have explored the effects of combining two drugs: trametinib, which inhibits KRAS signaling (a growth-promoting pathway that helps fuel many kinds of cancer) and hydroxychloroquine, which interferes with autophagy (the process by which cells salvage unwanted materials). Once the researchers determined that the combination reduced pancreatic tumors in mice, it was given to a patient who had exhausted other treatment options. The response was striking, extending the patient’s survival for eight months. After moving the experimental treatment from the lab to the clinic in just three years, Kinsey has launched a clinical trial, which will evaluate its effects across dozens of patients.
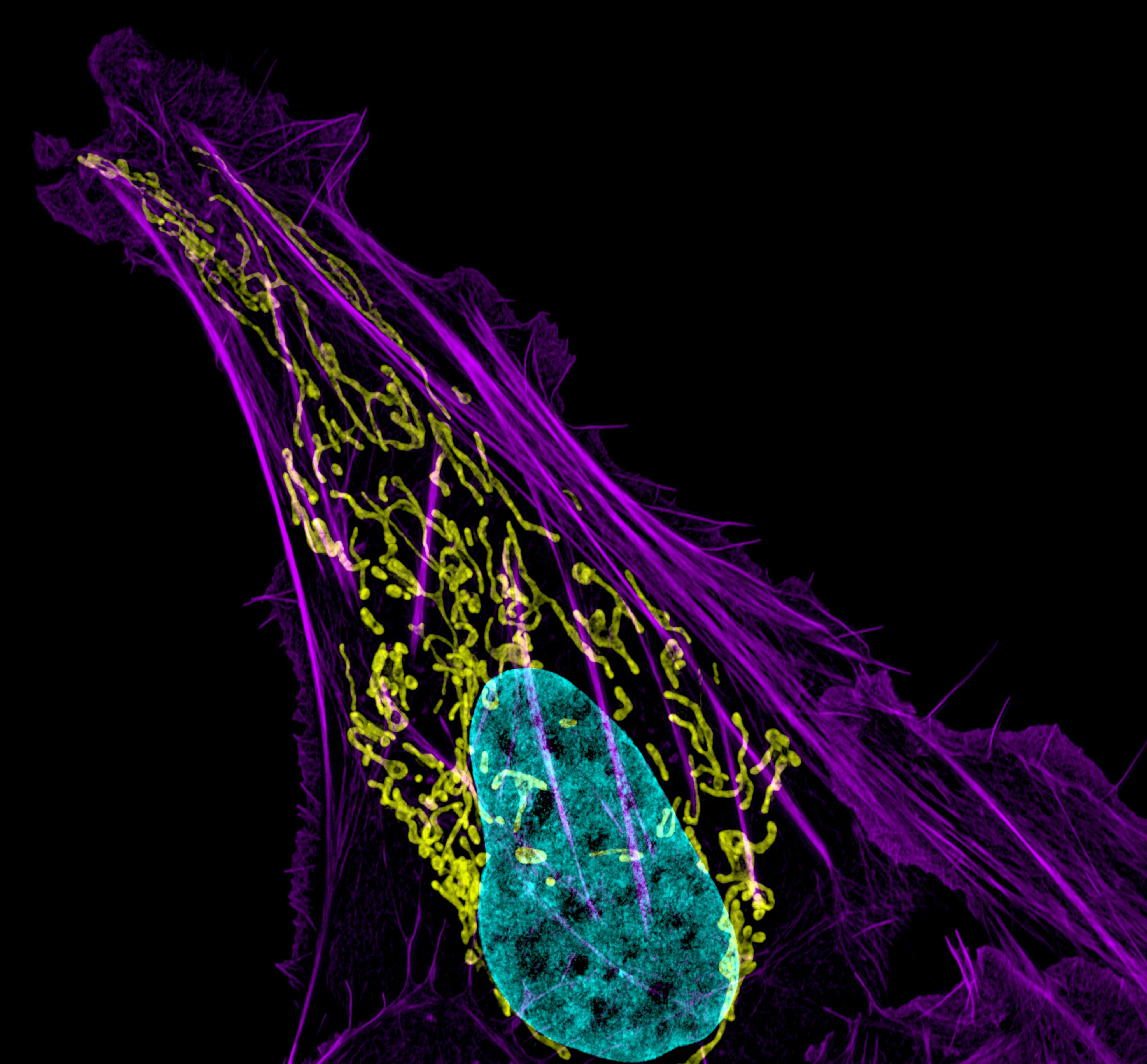
Many cancer patients are at risk for fractures due to bone loss. Sometimes, that bone loss is a side effect of treatment. It can also be triggered by cancer cells themselves. It’s a particular problem for patients with metastatic breast cancer, which frequently reaches the bones, breaking down existing tissue as new tumors form.
Cancer biologist Alana Welm, PhD, has identified a signaling protein called RON kinase that is activated by metastatic cancer cells to spur the breakdown of bone. In animal studies, blocking that protein prevents metastasis-driven bone destruction. Welm’s team has also found evidence of reduced bone turnover—a process that involves both bone loss and regrowth—among cancer patients who received an experimental RON kinase inhibitor in an early clinical trial. Based on their findings, the team believes drugs that interfere with RON kinase signaling could reduce bone loss in patients whose breast cancer has metastasized to the bone.
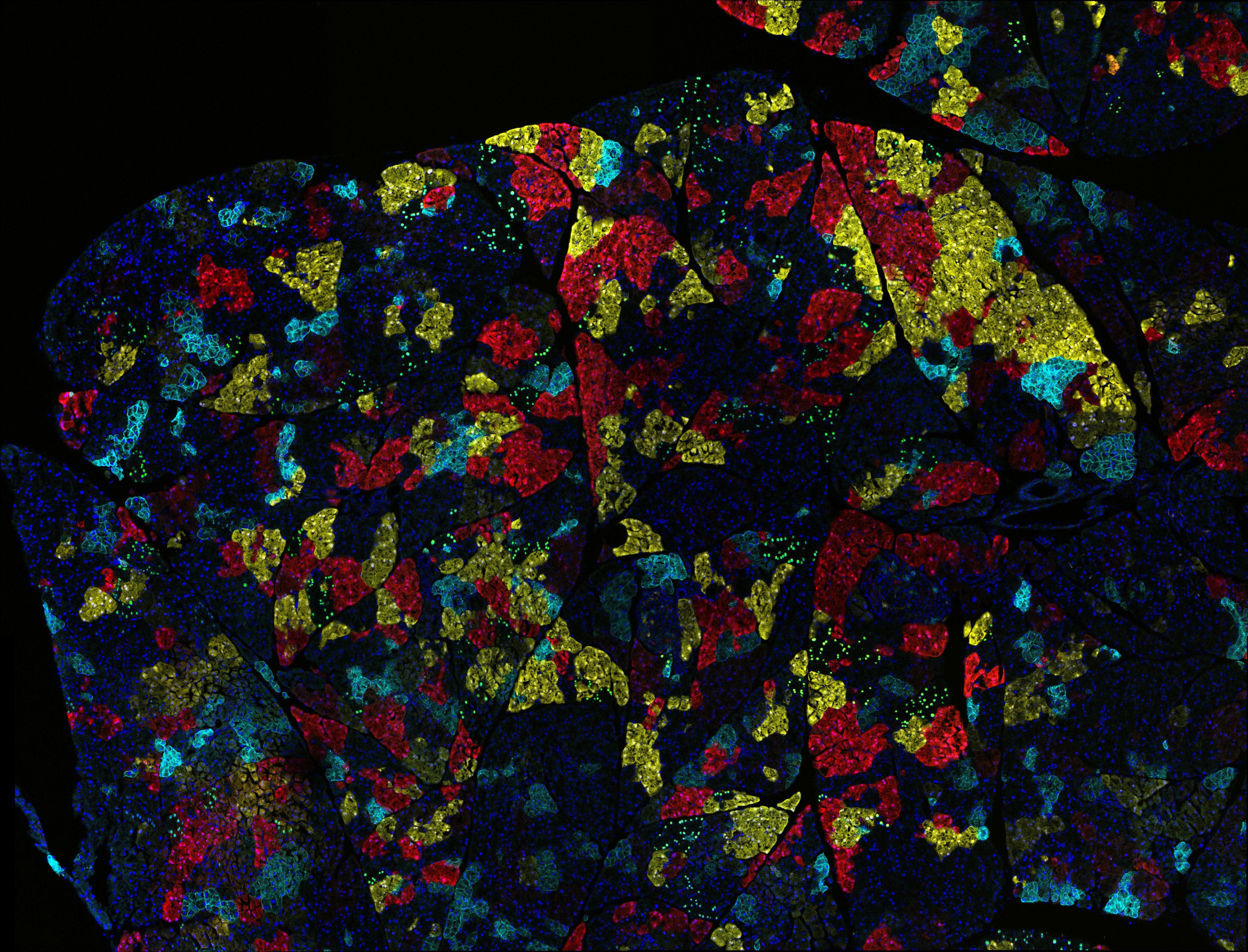
Non-small-cell lung cancers (NSCLC) are the most common form of lung cancer, and their prognosis is poor. Only 15 percent of patients with this disease survive five years past their diagnosis. Chemotherapy only works for about 30 percent of patients. Cancer immunotherapies can help some patients’ immune systems fight their tumors—but these, too, only work for a small fraction of people with NSCLC.
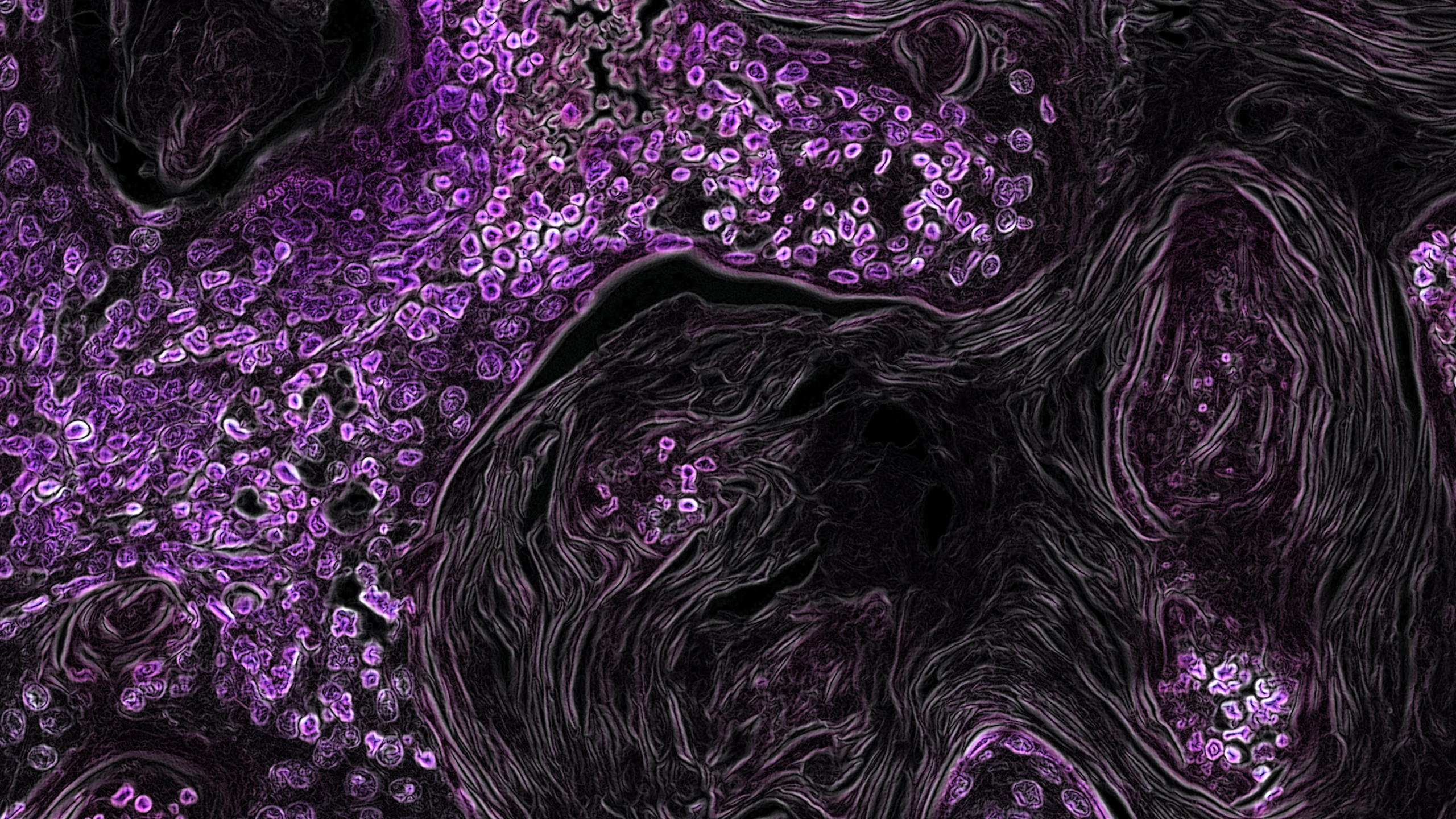
HCI investigator Trudy Oliver, PhD, thinks that in order to improve treatment options, it will be important to understand what drives different types of NSCLCs and how these cancers impact the immune system. Her team has developed a mouse model of one type of NSCLC, squamous cell carcinoma, and used it to show how overactive proteins in the tumor cells manipulate signaling to recruit immune-suppressing cells to their environment. The findings point to genes and pathways that may limit immunotherapy response and could help researchers find ways to overcome them.
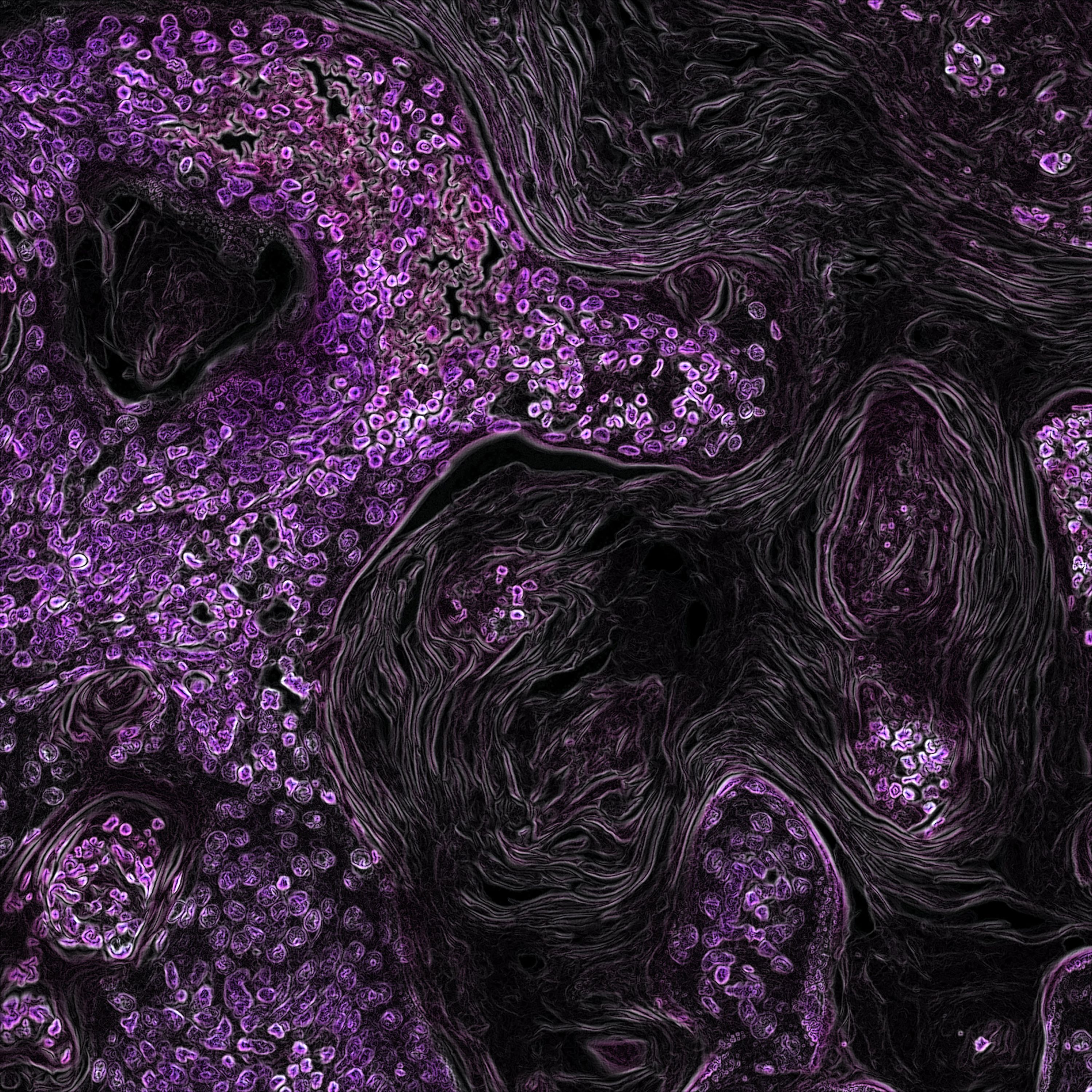
Women with triple-negative breast cancer usually undergo surgery to remove their tumor, before or after chemotherapy. The majority of patients respond well to this treatment, but for about 40 percent of patients, the cancer soon returns. Since there is no way to determine which patients are at greatest risk of relapse, almost everyone receives an aggressive chemotherapy regimen.
After analyzing tumor samples from women who had been treated for triple-negative breast cancer, cancer biologist Katherine Varley, PhD, and colleagues noticed that patients with the best outcomes had something in common: their tumor cells had switched on certain genes that made them more visible to the immune system. They found that by measuring the activity of 36 genes involved in immune activation, they could distinguish between patients whose disease recurred after treatment and those who remained cancer-free. With further validation, such an analysis might enable clinicians to assess individual risk and offer patients with triple-negative breast cancer more personalized treatment plans.
Pioneering the Future: Stories of Discovery & Innovation at University of Utah Health
Special thanks to Wes Sundquist and Alfred Cheung for their dedicated work compiling research discoveries.
Written by: Jennifer Michalowski
Editing by: Julie Kiefer
Layout and Design by: Kyle Wheeler
Production Supervision: Abby Rooney, Julie Kiefer, Kyle Wheeler
Supported by: Will Dere, Chris Hill, Amy Tanner