Pioneering the Future
Stories of Discovery & Innovation

Protecting Health Through Prevention
June 17, 2022
To keep people in good health, it’s always better to prevent problems from developing rather than dealing with issues once they arise. At U of U Health, researchers are exploring innovative approaches to prevent a wide range of conditions, from muscle loss to dangerous infections. Time and again, these researchers have demonstrated that preventive measures—including many that are inexpensive and easy to implement—are important and effective strategies for improving health.
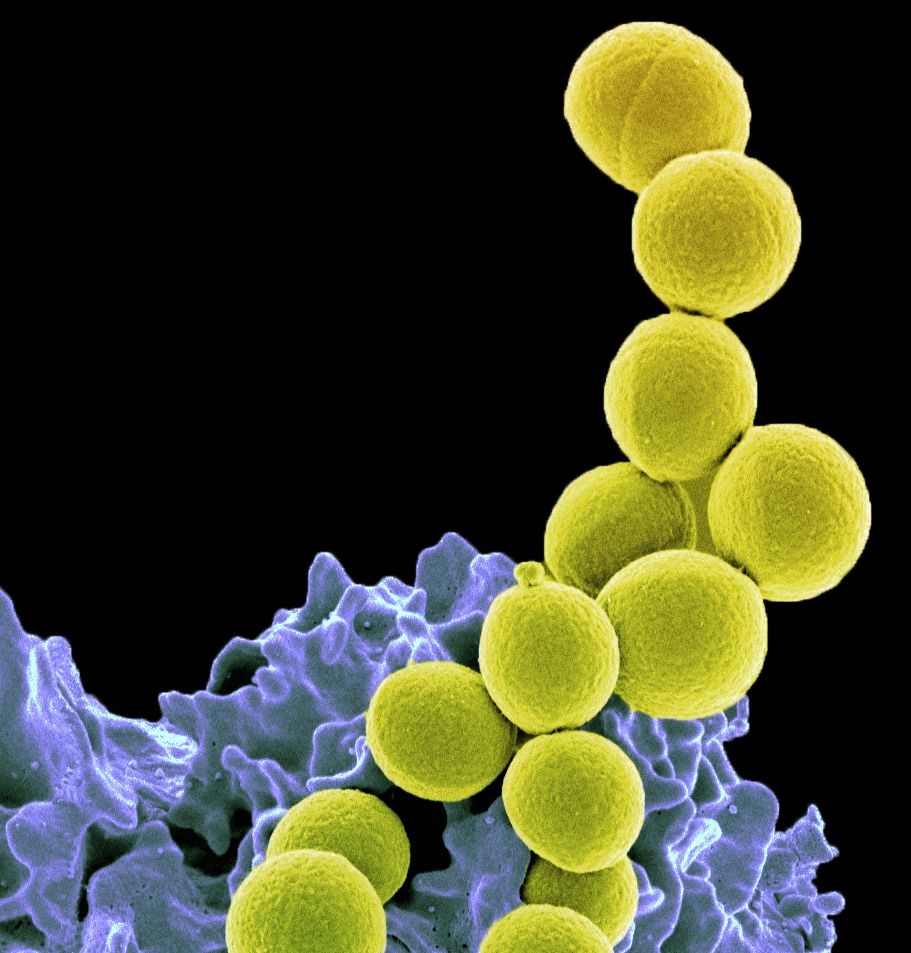
Methicillin-resistant Staphylococcus aureus (MRSA) is a type of bacteria that many people have on their skin or in their noses. Without control systems in place, it can spread easily within healthcare settings. This can pose serious problems because when the bacteria enter the body—often through a wound or surgical site or medical device—serious infection can develop. Because MRSA is resistant to many common antibiotics, these infections can be difficult and costly to treat.
Professors of epidemiology in the Department of Internal Medicine, Michael Rubin, MD, PhD, and Matthew Samore, MD, have shown that healthcare facilities can prevent MRSA infections with cost-effective procedures that control the bacteria’s spread. Research from their team tied declining rates of MRSA infection in Veterans Affairs hospitals to implementation of contact precautions—meaning healthcare workers wear gowns and gloves during their interactions with patients that were carrying the drug-resistant bacteria. In an analysis of more than 100 hospitals, their team found that these procedures cut MRSA transmission in half. Their studies demonstrate the importance of isolation procedures in preventing healthcare-associated infections, a strategy that has also proven critical during the pandemic for limiting the spread of COVID-19.
When it comes to muscle, it’s use it or lose it, particularly as we age. As people get older, it’s more likely that they will need periods of rest to recover from injuries or illness—and while prolonged inactivity can cause anyone’s muscles to atrophy, older people lose muscle more quickly. That can leave them more vulnerable to falls and injury once they’re ready to move again.
Researchers led by Micah Drummond, PhD, assistant professor of physical therapy and athletic training, compared how five days of bed rest impacted the muscles of adults in different age groups. They discovered that people in their 60s and 70s lost more muscle than younger adults not only because existing muscle proteins broke down more quickly but also because protein production in their muscle cells had slowed. They found they could preserve older individuals’ muscle mass during bed rest by combining two treatments that increase the production of new muscle proteins: dietary protein supplementation and electrical stimulation of inactive muscles. These findings will help develop strategies that protect older adults’ muscle function during periods of disuse.
Emergency contraception prevents pregnancy after unprotected sexual intercourse. The most effective method of emergency contraception is an intrauterine device (IUD). Copper IUDs, highly effective as routine birth control, were the first type of IUD recognized as an effective form of emergency contraception. But people more frequently prefer the hormonal IUD over the copper because it so effectively reduces or eliminates menstrual bleeding and cramping.
David Turok, MD, MPH, associate professor of obstetrics and gynecology, and colleagues were the first to evaluate a hormonal IUD for emergency contraception. In a randomized study involving hundreds of people published in the New England Journal of Medicine, they found that the levonorgestrel IUD, which contains a synthetic version of the hormone progesterone, is no less effective than the copper IUD for pregnancy prevention after unprotected intercourse. As a result, levonorgestrel IUD has been approved for this use by all 600+ Planned Parenthood clinics nationwide. “This is all about increasing access and options for people,” Turok says.
Understanding what triggers a child’s asthma can help doctors and families figure out how to prevent attacks. Ideally, doctors would adjust medications and tailor their recommendations based on a patient’s potential exposure to asthma triggers. But so many factors—from air pollution to infection to stress—can drive attacks of the airway-restricting disease that clinicians rarely have enough information to provide a truly personalized treatment plan.
Led by Kathy Sward, PhD, professor in the College of Nursing, and Julio Facelli, PhD, distinguished professor in the Department of Biomedical Informatics, U of U Health scientists spent years developing an online platform where kids with asthma, parents, doctors, and researchers can feed real-time information into a comprehensive database. Their system is designed to integrate data from both regional and personal air quality monitors with clinical information from doctors’ records and emergency room visits. Tracking an individual’s “exposome” is expected to both improve individual patient care and provide a rich source of data for asthma researchers.

Pioneering the Future: Stories of Discovery & Innovation at University of Utah Health
Special thanks to Wes Sundquist and Alfred Cheung for their work to compile the discoveries and innovations that make this series possible.
Written by: Jennifer Michalowski
Editing by: Julie Kiefer
Layout and Design by: Kyle Wheeler
Production Supervision: Abby Rooney, Julie Kiefer, Kyle Wheeler
Supported by: Will Dere, Chris Hill, Amy Tanner