Pioneering the Future
Stories of Discovery & Innovation
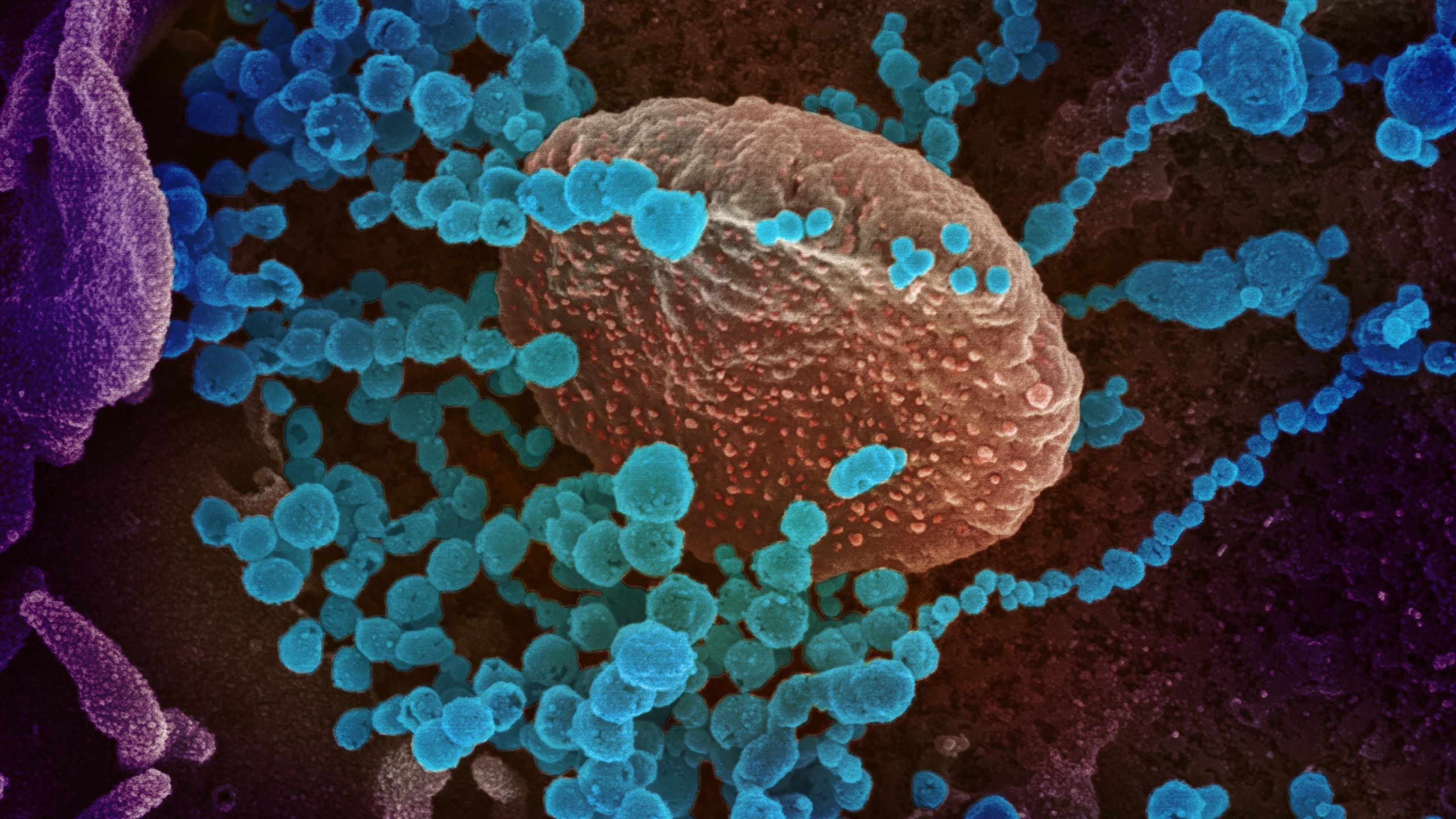
Combating COVID-19
March 18, 2022
The virus that causes COVID-19 first emerged in 2019, and it wasn’t long before it was clear that the new pathogen would have a devastating effect on global health. Scientists around the world responded quickly, redirecting their research to address the growing pandemic. At University of Utah Health, many were able to build on knowledge from prior studies of the immune system to begin figuring out how the body responds to infection with SARS-CoV2, and why some cases become life-threatening. Meanwhile, bioengineers worked on another front, increasing availability of critical medical equipment when it was in short supply.
In severe cases of COVID-19, the body’s immune response to the virus can be catastrophic, triggering excessive inflammation and life-threatening blood clots. Lung damage is exacerbated when immune cells called neutrophils release sticky, toxic webs called NETs, which are useful for killing pathogens but may harm the body’s own tissues, as well.
U of U Health investigators Christian Yost, MD, Guy Zimmerman, MD, and colleagues have studied how NETs are released and how their dysregulation contributes to disease. Once they realized that the most dangerous COVID-19 complications seemed to be driven by the body’s immune response to infection, they began to suspect NETs might be involved. Working with pulmonologist Elizabeth Middleton, MD, and others, they linked excessive NET production to the pneumonia and acute respiratory distress syndrome that can occur when COVID-19 is severe. Blocking NET formation is now being explored as a potential strategy for treating COVID-19.
Dysregulated NET formation is not limited to cases of serious COVID-19. The phenomenon occurs in a host of inflammatory syndromes and may similarly serve as a therapeutic target for those conditions.
Blood clots are a dangerous complication of COVID-19. Untreated, they can cause life-threatening strokes, heart attacks, or pulmonary embolism. These conditions are most common in patients with severe COVID-19, but milder cases also seem to increase the risk of blood clots.
Clots form when platelets in the blood stick together. So when it became clear early in the pandemic that clots were contributing significantly to mortality among patients with COVID-19, U of U Health scientists Robert Campbell, PhD, and Matthew Rondina, MD, and colleaguesstudied the platelets of people hospitalized with the disease. They found that infection with SARS-CoV-2 triggers changes in platelets’ genetic activity that makethe cells more prone to clotting. Hyperactive platelets may also help drive inflammation in the lungs of people with severe COVID-19, worsening respiratory distress.At the same time, platelets participate in the immune system’s antiviral response. Understanding platelets’ role in the illness led researchers to begin exploring antiplatelet therapies as a treatment for COVID-19 and a variety of common thrombotic conditions.
At the beginning of the COVID-19 pandemic, hospitals around the world were concerned that they would not have enough ventilators to care for patients in need. To address this dire situation, U of U Health bioengineer Kai Kuck, PhD, collaborated with colleagues at Stanford and Brown Universities to develop a low-cost, easy-to-manufacture, intensive-care ventilator.
The result was the Pufferfish ventilator, which can deliver high-flow oxygen therapy and mechanical ventilation. Plans for Pufferfish’s manufacture and distribution were developed in partnership with teams in Nepal, Kenya, and India, and prototypes reached communities around the world by the summer of 2020. To empower communities to build their own Pufferfish, the development team shared its design plans freely and ensured that the ventilator could be assembled quickly with readily available materials, without relying on strained medical supply chains. The shared resource will benefit communities not only during surges of COVID-19 but also when there is an urgent need to support patients with other forms of pneumonia and respiratory failure.

Pioneering the Future: Stories of Discovery & Innovation at University of Utah Health
Special thanks to Wes Sundquist and Alfred Cheung for their work to compile the discoveries and innovations that make this series possible.
Written by: Jennifer Michalowski
Editing by: Julie Kiefer
Layout and Design by: Kyle Wheeler
Production Supervision: Abby Rooney, Julie Kiefer, Kyle Wheeler
Supported by: Will Dere, Chris Hill, Amy Tanner



