Fighting the Opioid Epidemic— A Plague on All Our Houses
December 14, 2020
In fewer than 25 years, opioid addiction has devastated the United States. Nearly 450,000 people have died from an overdose caused by prescription or illicit drugs. Each of those deaths represents an individual tragedy. Taken together, it represents a social epidemic staggering in its toll.
Between 2015 and 2018 alone, the economic impact of this epidemic reached a staggering $2.5 trillion in unexpected mortality, lost productivity, increased health care and criminal justice costs, and child education assistance. In 2020, with the COVID-19 pandemic raging, data shows that overdose deaths are rising as people struggle with social isolation, job loss, and stress. Now, it’s time for health care systems to work with community partners to address this epidemic with holistic solutions that address a diverse array of needs—from life-saving interventions to the management of chronic conditions.
Two truths we need to accept: Opioid addiction isn’t a moral failure, and it affects people from all walks of life. The newlywed who overdosed after becoming addicted to pain pills prescribed for a tonsillectomy. The young mother who hoped Percocet could help with her postpartum depression. The upstanding school superintendent and church bishop. The religious couple who met in recovery. And Stephanie, who, after many failed attempts to kick her lifelong addiction, finally found the combination of resources she needed.
Stephanie* lay in the Salt Lake County Metro Jail bunk bed and thought, “Everything would be better if I just died.”
She was a burden to everyone she knew, she thought, and no one could trust her. She’d pawned her mom’s wedding ring, stolen her sister’s jewelry. There was nothing she wouldn’t do—or steal—to stave off the desperation, seizures, and overwhelming sickness that assaulted her body every time she was “jonesing.”
Sexually molested and raped as a child, she’d started using drugs at age 13 while growing up in Springville and Provo. It wasn’t until she went to prison for drug-related crimes that she decided she wanted to change, not die.
But after taking up healthy habits and being released, she realized that transitioning back into society was more difficult than she expected. After a stint in the Orange Street halfway house for women, she lived in a tiny apartment with only a blanket and pillow while working as a server in a Mexican restaurant.
She met her husband, also a recovering addict, while riding TRAX. They relied on Suboxone (buprenorphine/naloxone), a medication used in opioid replacement therapy. But the couple relapsed. Two more stints in prison and still Stephanie and her partner couldn’t figure out how to turn their lives around. When she found herself pregnant, she was terrified the state would take her baby away. Her doctor told her to aggressively taper the medication, but that only led to more cravings.
*Stephanie requested anonymity to share her story.
How did a woman like Stephanie end up affected by the opioid epidemic? Through a complicated matrix of reasons resulting from the missteps of the very health care system now tasked with solving it. In the 1990s, doctors began prescribing opioids more widely when patient surveys revealed an inability to control their pain. At the same time, a new wave of opioids were being aggressively marketed as safe and non-addictive painkillers. By 2012, doctors prescribed more than 255 million opioids nationwide. Today, roughly 25 percent of the patients prescribed those opioids misuse them.
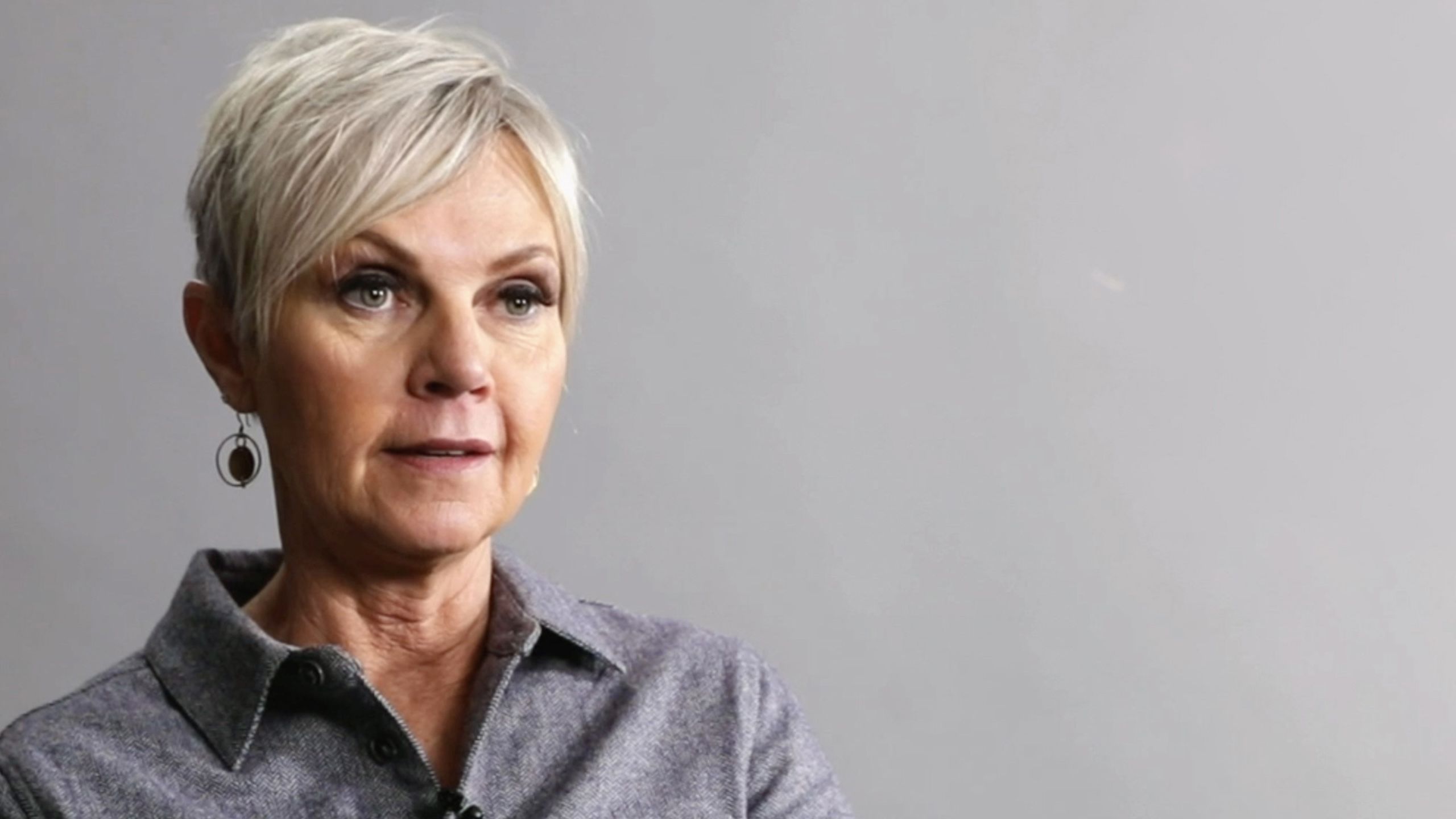
Opioid addiction obliterates distinctions between gender and socioeconomic status. Here in Utah, it affects BYU football players, mid-career professionals, new moms, and 20-somethings alike, as evidenced by the recovery stories highlighted on the next page. And yet we still haven’t reckoned with the extent of the epidemic. “Addiction has been constructed as a social problem,” says Marcela Smid, MD, MS, MA, an assistant professor in the Division of Maternal-Fetal Medicine and the medical director of U of U Health’s Substance Use in Pregnancy Recovery Addiction Dependence (SUPeRAD), a specialty prenatal clinic for women with substance abuse issues. “Medicine is catching up to the fact that addiction is truly a life-threatening chronic condition.”
Marcela Smid, MD, MS, MA. Photo by Corrin Rausch, ARUP.
Marcela Smid, MD, MS, MA. Photo by Corrin Rausch, ARUP.
No magic pill can reverse the damage done by the trillions of pills prescribed and consumed over the last 25 years. But removing the stigma of addiction is an important first step—followed by outreach programs, clinical education, and cutting-edge research aimed at tackling opioid addiction like any other scientific conundrum in urgent need of a solution.
When Smid and her colleagues studied every drug-induced, pregnancy-associated death in Utah from 2005-14, their findings were chilling. None of the women received social work consultation or mental health services before their deaths—even though 1 in 5 of them had previously attempted suicide. None were screened for drug use. And none had received pharmacotherapy to manage their opioid use disorder.
Stephanie was one of the lucky ones. She connected with Smid at the SUPeRAD clinic and told her about her reliance on Suboxone. “I need to get off this,” she told Smid, who pleaded with her: “Don’t do anything. Stay on it. You’re stable on the medication, and that is the most important thing you can do for you and your baby.”
FROM 1999-2019:
the number of opioids
prescribed per person
in the United States
tripled
In 2018, alone
1.8 million opioid prescriptions
were dispensed in Utah
— enough to give a
bottle of pills to
82%
of all Utah adults
In 2020 alone,
the opioid epidemic is
projected to cost
$500B
nationwide
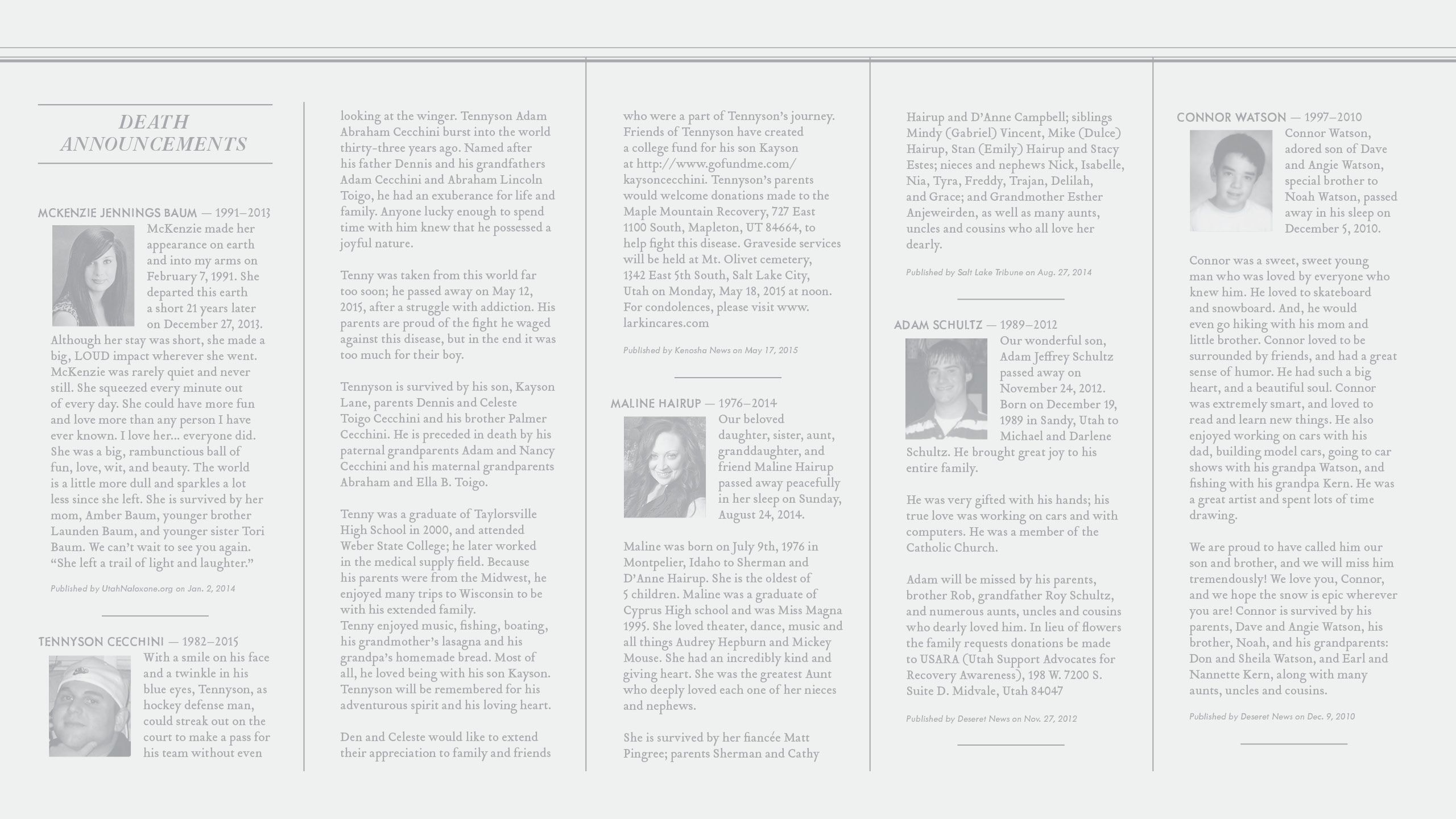
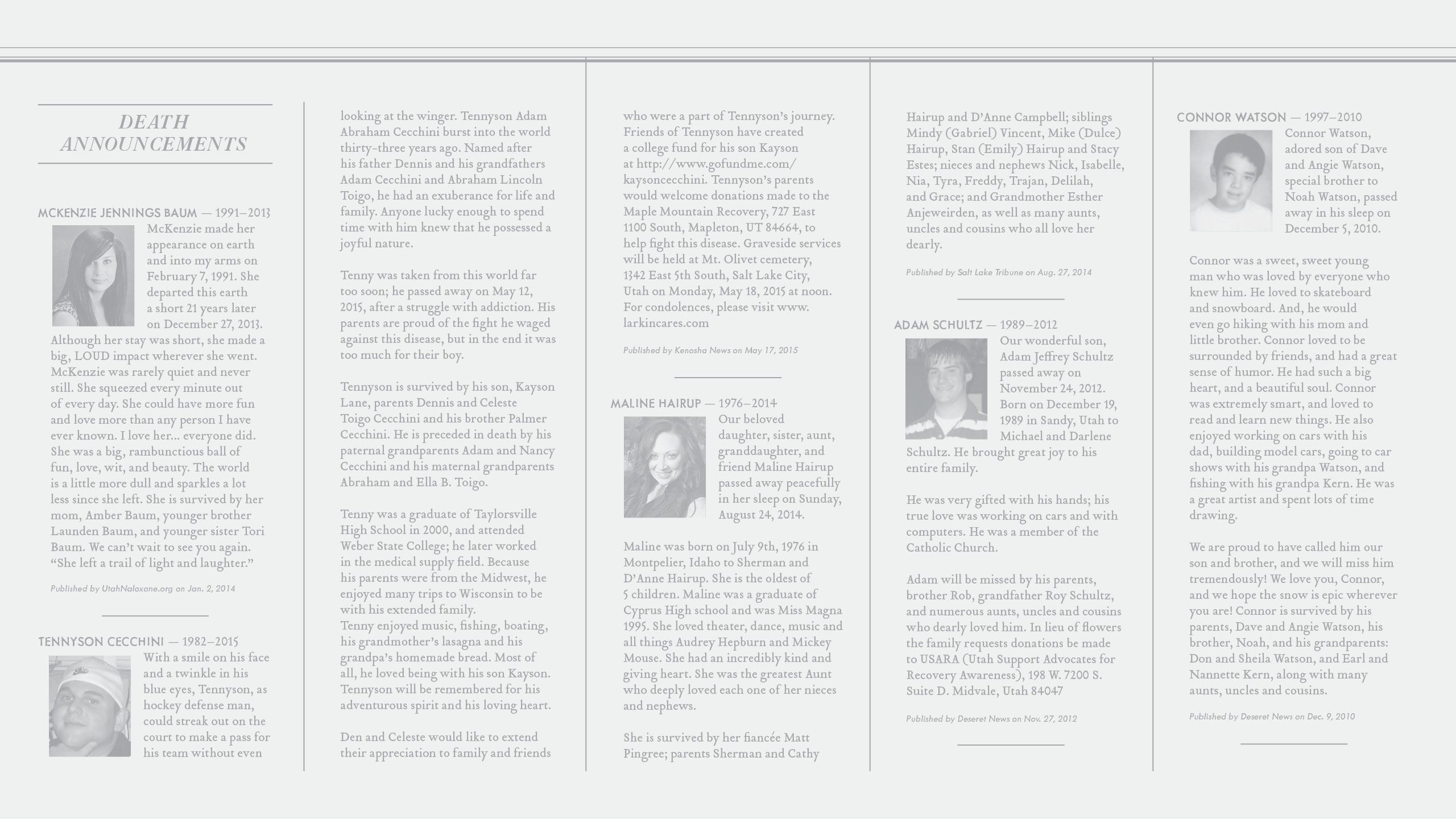
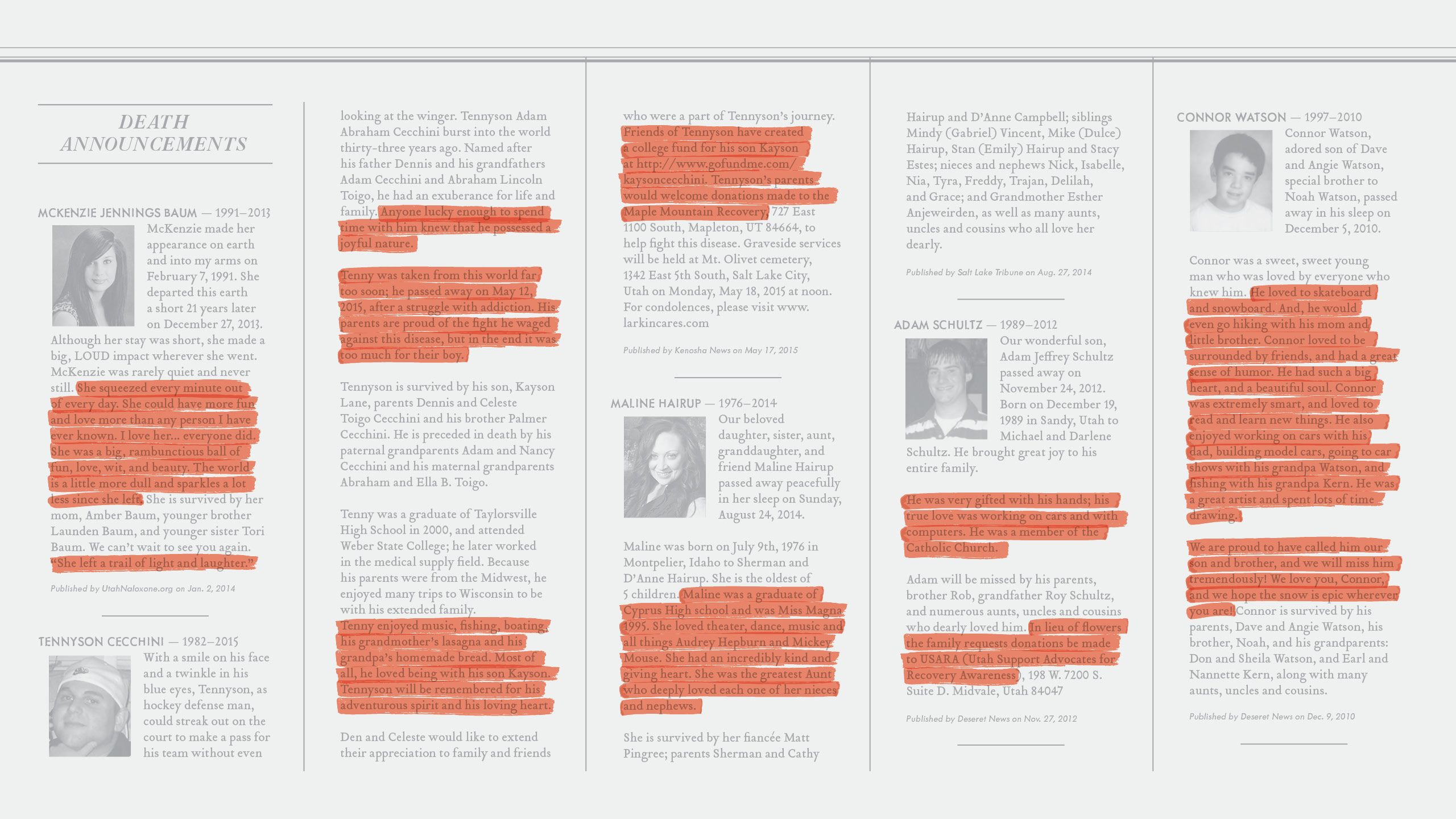
STORIES OF RECOVERY
End the Stigma. Start the Conversation. Stop the Epidemic.
These stories of recovery are shared, with permission, from the Stop the Opidemic campaign, a joint venture between local, state, national, nonprofit, and university partners. Find out more at stoptheopidemic.org.
Dennis and Celeste, SLC: “Our son died at 33 from a heroin overdose. He was a wonderful skater and hockey player, but he hurt his shoulder—and the doctor gave him opioids for the pain. We were completely oblivious to his problems, but once we found out he was addicted, it was complete and utter panic. And that panic stemmed from not even understanding how to help him.”
Alema, Sandy: “I played football at BYU, where I was first exposed to opioids. I went from trying Percocet to spiraling out of control and buying heroin on the street. There’s so much shame associated with that, but I had to be humble enough to ask for help: ‘I have a disease. Without treatment, it will kill me. But it’s treatable.’”
Cris, Ogden: “I still struggle saying my son is an addict. He had two surgeries after we knew, and I told him, ‘Don’t tell the orthopedic surgeon that you’re addicted to anything.’ What was I thinking? It’s like you want to keep this awful, evil secret to yourself, which helps no one. It doesn’t help your kid. It doesn’t help you change society.”
Lizzy, Mountain Green: “I worked as a registered nurse up until I had my daughter. Three weeks later, the postpartum depression set in. I had a wicked headache, so I took the pain medication. Within a month and a half, I started to lie to my husband. I stole some pills from a family member. Then I entered treatment. The most Christ-like people in this whole world are in recovery. They’re truly living the atonement—the process of repentance.”
Amy, SLC: “I did everything society told me to do. I went to college, got married in my church, succeeded in my career. Then, that opioid took me down. It took everything. I was a shell—just another homeless person on the streets. After seven different times in jail, I got into treatment. And it’s only because of that program that I’m alive today and embedded in the SUPeRAD clinic as a residential treatment liaison. You are not what you’ve done—you are what you’ve overcome.”
Images courtesy of Stop the Opidemic




STORIES OF RECOVERY
End the Stigma. Start the Conversation. Stop the Epidemic.
These stories of recovery are shared, with permission, from the Stop the Opidemic campaign, a joint venture between local, state, national, nonprofit, and university partners. Find out more at stoptheopidemic.org.
Dennis and Celeste, SLC: “Our son died at 33 from a heroin overdose. He was a wonderful skater and hockey player, but he hurt his shoulder—and the doctor gave him opioids for the pain. We were completely oblivious to his problems, but once we found out he was addicted, it was complete and utter panic. And that panic stemmed from not even understanding how to help him.”
Alema, Sandy: “I played football at BYU, where I was first exposed to opioids. I went from trying Percocet to spiraling out of control and buying heroin on the street. There’s so much shame associated with that, but I had to be humble enough to ask for help: ‘I have a disease. Without treatment, it will kill me. But it’s treatable.’”
Cris, Ogden: “I still struggle saying my son is an addict. He had two surgeries after we knew, and I told him, ‘Don’t tell the orthopedic surgeon that you’re addicted to anything.’ What was I thinking? It’s like you want to keep this awful, evil secret to yourself, which helps no one. It doesn’t help your kid. It doesn’t help you change society.”
Lizzy, Mountain Green: “I worked as a registered nurse up until I had my daughter. Three weeks later, the postpartum depression set in. I had a wicked headache, so I took the pain medication. Within a month and a half, I started to lie to my husband. I stole some pills from a family member. Then I entered treatment. The most Christ-like people in this whole world are in recovery. They’re truly living the atonement—the process of repentance.”
Amy, SLC: “I did everything society told me to do. I went to college, got married in my church, succeeded in my career. Then, that opioid took me down. It took everything. I was a shell—just another homeless person on the streets. After seven different times in jail, I got into treatment. And it’s only because of that program that I’m alive today and embedded in the SUPeRAD clinic as a residential treatment liaison. You are not what you’ve done—you are what you’ve overcome.”
Images courtesy of Stop the Opidemic
Smid compares addiction to one of America’s most common afflictions—type 1 diabetes. Roughly 10–20 percent of patients with both chronic diseases can stop taking their meds cold turkey and be fine. But the vast majority, like Stephanie, need other medication for the rest of their lives to stabilize their brain. “Their bodies lack natural endorphins,” Smid says. “If more people thought about addiction like diabetes, we’d be in a better place.”
Smid trains university clinicians to ask—and to listen. She encourages them to use the National Institute on Drug Abuse Quick Screen, a questionnaire about substance use that broaches the potentially sensitive topic of prescription and opioid misuse. Some providers see it as another list of inconvenient questions. But Smid sees it as a simple intervention that could save lives.
“Every provider needs to be screening all of their patients and not assuming they know what they’re doing based on how they look, how much money they have, or where they live,” Smid says. “We don’t have an opioid epidemic; we have a pandemic. It’s not poor, middle-class, or rich people—it’s all people.”
Everyone struggling with addiction deserves that kind of attention, says Jennifer Plumb, MD, MPH, associate professor in the Department of Pediatrics and medical director of Utah Naloxone, which recently launched a free wellness center and clinic in downtown SLC—the first of its kind in Utah—to help those impacted by substance use.
The clinic offers syringe exchange, HEP C/HIV/STI testing, patient navigation, referrals to Smid’s SUPeRAD clinic, and peer support from coaches at Utah Support Advocates for Recovery Awareness (USARA).
“Our partnership with U of U Health has been significant,” says Mary Jo McMillen, director at USARA. “Clinicians invite our coaches into a medical environment where they meet patients at a place of common lived experience.” Evan Done, development director at USARA, adds, “We try to keep people engaged. After acute care is delivered, USARA steps in to help patients manage their lifelong medical condition.”
That approach worked for Stephanie. In 2019, she delivered a healthy baby; she has maintained the same steady dose of Suboxone for three years. Because Smid treated her addiction without judgment—instead of aggressively acting to end it—Stephanie now has the stability she needs. “This is like my fifteenth chance, and I’m very grateful where I am right now,” she says. “I’m in a better place than I have been since I was 10 years old.”
FROM 1999-2019:
Prescription opioid
overdoses killed
more than
232K
Americans
Utah has ranked
top 10
in the nation for
overdose deaths
over the last 10 years
From 2000–2015, Utah
experienced a nearly
400%
increase in deaths
from the misuse and abuse
of prescription drugs
Seeking New Solutions Underwater Researchers are looking for the next source of non-opioid painkillers in an unexpected place: tropical oceans. In locations as far-flung as the Philippines (shown here), the Caribbean Sea, the Solomon Islands, and the Gulf of Mexico, fishermen like Jose Arbasto (right) and scientists like Iris Bea Ramiro, BSc (left) work together to collect Conus regius. Photos by Helena Safavi-Hemami.
Seeking New Solutions Underwater Researchers are looking for the next source of non-opioid painkillers in an unexpected place: tropical oceans. In locations as far-flung as the Philippines (shown here), the Caribbean Sea, the Solomon Islands, and the Gulf of Mexico, fishermen like Jose Arbasto (right) and scientists like Iris Bea Ramiro, BSc (left) work together to collect Conus regius. Photos by Helena Safavi-Hemami.
The cone snail's venom has led to breakthroughs in both opioid treatment and mini-insulin, offering a way to make prescription drugs as effective as opioids—but without addictive properties. Photo by Helena Safavi-Hemami.
The cone snail's venom has led to breakthroughs in both opioid treatment and mini-insulin, offering a way to make prescription drugs as effective as opioids—but without addictive properties. Photo by Helena Safavi-Hemami.
After five years as a researcher at University of Utah, Helena Safavi-Hemami, PhD, took a new position at the University of Copenhagen. U of U research colleagues, including Baldomero Olivera, PhD, are continuing the work synthesizing potentially analgesic properties and compounds in the snail’s venom. Photo courtesy Helena Safavi-Hemami.
After five years as a researcher at University of Utah, Helena Safavi-Hemami, PhD, took a new position at the University of Copenhagen. U of U research colleagues, including Baldomero Olivera, PhD, are continuing the work synthesizing potentially analgesic properties and compounds in the snail’s venom. Photo courtesy Helena Safavi-Hemami.
ATTACKING ADDICTION FROM ALL ANGLES
RESEARCH-DRIVEN SOLUTIONS FROM ACROSS ACADEMIA
From basic biology and population health to community connections, interdisciplinary researchers innovate to bring about real change in the opioid crisis.
PRESCRIBING FEWER OPIOIDS
Utah providers are taking responsibility, reducing the number of prescriptions written per 100 persons by 30% between 2008 to 2017. University of Utah Medical Group is building analytics to scale this success up to a system level.
ALTERNATIVE APPROACHES
Low back pain is a leading contributor to the prescription of opioid painkillers. But studies show that opioid treatments lead to more adverse medication-related events while failing to benefit pain-related function. A large clinical trial conducted by therapists, providers, and biostatisticians helps clinicians develop personalized treatment plans that reduce pain intensity with non-opioid treatment.
AT-HOME DISPOSAL
Up to 90 percent of patients don’t finish their opioid prescriptions, and many fail to dispose of extra medication. A pilot study armed patients with a home disposal kit; after undergoing elective surgery, patients given kits were 20 percent more likely to dispose of their excess pills. The team is currently expanding the program to further reduce the number of opioids in circulation.
NEXT-GEN COMMUNICATIONS
Breakdowns in communication often lead to overprescription. Researchers are integrating recommendations from the CDC Guideline for Prescribing Opioids for Chronic Pain directly into electronic health records, a large-scale effort that can streamline information sharing and lower overall prescription rates.
IMPROVING CARE FOR VETERANS
Veterans with mental health disorders receive opioids for pain diagnoses three times more than veterans without. The Program for Addiction Research, Clinical Care, Knowledge, and Advocacy (PARCKA) Vulnerable Veteran—Innovative Patient Aligned Care Team (VIP) Initiative embeds addiction care within primary care and improves acceptance among patients who cannot, or will not, seek it through more traditional mental health care settings.
ATTACKING ADDICTION FROM ALL ANGLES
RESEARCH-DRIVEN SOLUTIONS FROM ACROSS ACADEMIA
From basic biology and population health to community connections, interdisciplinary researchers innovate to bring about real change in the opioid crisis.
Researchers are searching for the next source of non-opioid painkillers in an unexpected place: tropical waters in the Philippines (shown here), the Caribbean Sea, the Solomon Islands, and the Gulf of Mexico. Fishermen like Jose Arbasto (right) and scientists like Iris Bea Ramiro, BSc (left) work together to collect Conus regius. Photo by Helena Safavi-Hemami.
Researchers are searching for the next source of non-opioid painkillers in an unexpected place: tropical waters in the Philippines (shown here), the Caribbean Sea, the Solomon Islands, and the Gulf of Mexico. Fishermen like Jose Arbasto (right) and scientists like Iris Bea Ramiro, BSc (left) work together to collect Conus regius. Photo by Helena Safavi-Hemami.
The cone snail's venom has led to breakthroughs in both opioid treatment and mini-insulin, offering a way to make prescription drugs as effective as opioids—but without addictive properties. Photo by Helena Safavi-Hemami.
The cone snail's venom has led to breakthroughs in both opioid treatment and mini-insulin, offering a way to make prescription drugs as effective as opioids—but without addictive properties. Photo by Helena Safavi-Hemami.
After five years as a researcher at University of Utah, Helena Safavi-Hemami, PhD, took a new position at the University of Copenhagen. U of U research colleagues, including Baldomero Olivera, PhD, are continuing the work synthesizing potentially analgesic properties and compounds in the snail’s venom. Photo courtesy Helena Safavi-Hemami.
After five years as a researcher at University of Utah, Helena Safavi-Hemami, PhD, took a new position at the University of Copenhagen. U of U research colleagues, including Baldomero Olivera, PhD, are continuing the work synthesizing potentially analgesic properties and compounds in the snail’s venom. Photo courtesy Helena Safavi-Hemami.
PRESCRIBING FEWER OPIOIDS
Utah providers are taking responsibility, reducing the number of prescriptions written per 100 persons by 30% between 2008 to 2017. University of Utah Medical Group is building analytics to scale this success up to a system level.
ALTERNATIVE APPROACHES
Low back pain is a leading contributor to the prescription of opioid painkillers. But studies show that opioid treatments lead to more adverse medication-related events while failing to benefit pain-related function. A large clinical trial conducted by therapists, providers, and biostatisticians helps clinicians develop personalized treatment plans that reduce pain intensity with non-opioid treatment.
AT-HOME DISPOSAL
Up to 90 percent of patients don’t finish their opioid prescriptions, and many fail to dispose of extra medication. A pilot study armed patients with a home disposal kit; after undergoing elective surgery, patients given kits were 20 percent more likely to dispose of their excess pills. The team is currently expanding the program to further reduce the number of opioids in circulation.
NEXT-GEN COMMUNICATIONS
Breakdowns in communication often lead to overprescription. Researchers are integrating recommendations from the CDC Guideline for Prescribing Opioids for Chronic Pain directly into electronic health records, a large-scale effort that can streamline information sharing and lower overall prescription rates.
IMPROVING CARE FOR VETERANS
Veterans with mental health disorders receive opioids for pain diagnoses three times more than veterans without. The Program for Addiction Research, Clinical Care, Knowledge, and Advocacy (PARCKA) Vulnerable Veteran—Innovative Patient Aligned Care Team (VIP) Initiative embeds addiction care within primary care and improves acceptance among patients who cannot, or will not, seek it through more traditional mental health care settings.
More than
60
projects
Led by
100+
researchers
Across
26
departments
Housed in
7
University of Utah
schools and colleges
Raised
$45M
in funding
In conjunction with
33
state, national, and
international partners
All with
1
goal in mind:
ending the opioid epidemic
“Fighting the Opioid Epidemic—A Plague on All Our Houses”
Words by Nick McGregor with Stephen Dark
Design by
Jesse Colby
Extra thanks to
Julie Kiefer, Nafisa Masud, Katie McMinn and the Utah Department of Health, Angie Castor, the Cecchini family, Mindy Vincent, and the Schultz family.













